
Stroke survivor reflects on how her ‘superpower’ has shaped who she is today
When Bridie Kirsopp woke up with a severe headache, which quickly developed into a blurred vision, vomiting, and leaving her unable to stand up, she knew she wasn’t well, but at 17, couldn’t possibly have guessed she was having a stroke.
Neither did her doctors, but five days later, a CT scan revealed she had a clot on her brain.
“I just never thought it could happen to someone so young,” said the fashion blogger, from Leeds, West Yorkshire.
Although Bridie, now 29, only spent a week in hospital, after she finally called an ambulance in December 2012, the clot dispersed with treatment, but twelve years on she is still suffering from severe physical and psychological side effects of the stroke.
She said: “When my pain is at its worst, that’s when I can’t bear anything touching me or I can’t use my hand."
Immediately after her stroke, Bridie was left with severe fatigue and weakness on the left side of her body which, after a few months, developed into severe pain that “burnt from head to toe”.
Bridie explained she was offered no help to deal with the symptoms which she battled with daily.
“I was just such an anomaly without any proper support; you’re never told you’re going to have a stroke at 17 and no one else believes you can have one either,” Bridie said.
“I didn't understand enough about strokes or the chronic pain condition I was left with. Looking back, I was quite naive and fearful and that played havoc on my anxieties.”
The severe side effects meant Bridie couldn’t enjoy being a teenager or do what her friends were doing as she entered her twenties.
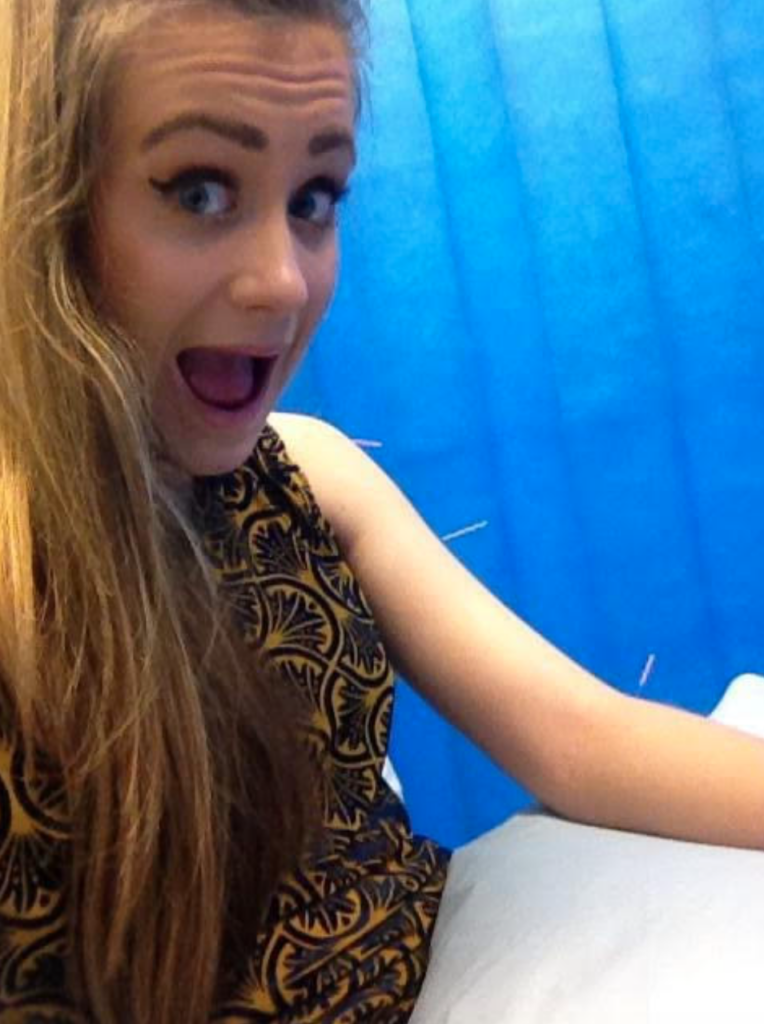
She said: “I was just so caught up in healing and controlling my pain. I didn't have time nor the good health to do the normal teen things like parties, dating and university. It’s all I've known through my most important years.”
Bridie, who will celebrate her 30th birthday next month, feels she has missed out on her youth and still has to manage how much she can do each day.
She said: “I don’t have any choice, I just need to limit myself and rest as much as I can.
“I still to make the mistake of taking too much on because I forget I don’t have a normal brain. I just need to listen to my body and accept it.”
As well as being left physically unable to do as much as her peers, Bridie’s psychological state has also suffered.
She said: “The mental impact has definitely been worse than the physical, and that is saying something with the debilitating pain I have.”
Bridie has undergone several years of psychotherapy to enable her to find a way of coping with everyday life, which includes never classing herself as a victim.
She said: “The word, victim, has negative connotations and puts emphasis on the suffering, making survivors seem weaker than they are. It puts the stroke above the person, even though they are doing all the work to get themselves back on their feet.
Bridie opts to use the term ‘survivor’ as a way of adapting to “her new self after trauma”.
She said: “I cannot imagine being me without my survivor identity. I've lost a lot, but gained so much more and I've figured out what truly matters in life.”
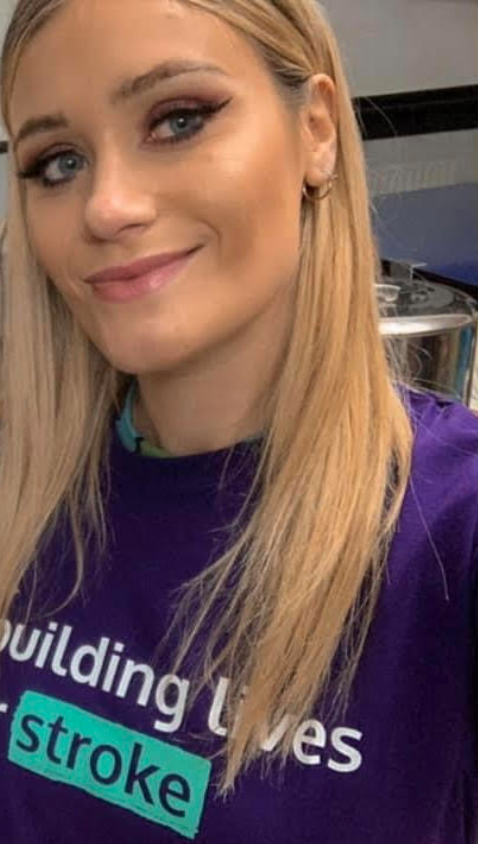
Bridie now works closely with Different Strokes, a charity helping young stroke survivors in the UK reclaim their lives.
Her neurologist introduced her to the charity after she had the stroke, but she didn’t get in touch with them until they were reintroduced in 2020.
She said: “I think I felt too ashamed. I didn't want to admit that I was now actually a stroke survivor, especially because I was so young.
“I quickly noticed a difference in how I see myself and it made me feel less alone and gave me a sense of purpose.
Bridie now feels after her stroke she is wiser, kinder, more receptive, and more open-minded.
“The biggest thing is my ability to feel deep compassion and advocate for what's right. Becoming marginalised completely changes you and your mindset.
“I feel like I've gained a superpower and I use it to my full advantage. The resilience I've carried has shaped me into the most authentic version of myself.”

Duty of Care: justified or flawed?
Next month, the legal duty of care for university students will be debated in parliament after a campaign was launched in September of last year.
The petition, which was brought by the #ForThe100 campaign group and received over 120,000 signatures, is aimed at improving mental health services in universities, in a bid to reduce the number of students taking their own lives, by calling for a statutory duty of care for students to be imposed.
At the moment, there is duty of care legislation in place for university staff as well as students under the age of 18.
ONS data revealed 64 university students took their own lives in the academic year ending 2020 in England and Wales. The campaign group believes this figure to be around 100.
Mike McCarthy, who helped create the suicide prevention charity, Baton of Hope, said: “If you’re under 35, man or woman, the biggest threat to your life is you. Not covid, cancer, drugs, road accidents, it’s you.”
While the aims of the petition are broadly agreed upon, there are concerns over privacy, funding and accountability with lecturers and university standards groups expressing their concerns about how this might be achieved.
What duties do universities have?
Currently, there is no legislative framework for universities and their duty of care toward their students. However, recommendations regarding a university’s approach to mental well-being and suicide have been made by Universities UK.
Professor Steve West CBE, President of Universities UK and Vice-Chancellor of UWE Bristol believes a statutory duty of care is not the correct approach to drive change and help in prevention and early intervention.
He said: “We do not believe the proposed additional statutory duty of care, beyond the existing duties that already apply to universities, would be practical, proportionate, or the best approach to supporting students.”
Sceptics of the legislative approach argue universities already provide mental well-being resources.
A spokesperson for the Department of Education, said: “We expect all universities to take active steps to prevent suicides and support students’ mental health.
“Every student death is a tragedy and we recognise that there are those with personal experience of these tragic events who have signed this petition, which will now be considered for debate in Parliament.”
A key point of contention between advocates and those expressing concerns about the proposed legislation is the belief that there already is an existing expectation of care, despite no legal mandate.
Georgina Calvert-Lee, a senior consultant and barrister at Bellevue Law, said: “Universities’ response is that they already do this, they don’t need to be mandated — but then why do they care if it’s a requirement, if they’re already complying?”
The legislation put forward by the petition already has support in Parliament from members who acknowledge the lack of a legal framework.
Tom Gordon, the Liberal Democrat Parliamentary Spokesperson for Harrogate and Knaresborough, said: "There is currently a lack of legal protections for students who don't benefit from the Equality Act and it is right that this should be changed."
Some advocates are pushing for more, though, claiming current services are not robust enough.
Mr McCarthy said: “The very clear picture that we get is that the support for students in terms of mental health provision and suicide prevention is inadequate — there’s no way to dress this up.”
The implications and concerns surrounding it
One of the biggest concerns surrounding the implementation of a duty of care legal mandate is accountability. Universities fear this might create an avenue to unjustly punish, not only institutions but also individual staff.

Dr Mark Shanahan is a politics lecturer who has been advocating for duty of care in higher education since his son, Rory, took his own life in 2018 when he was studying at the University of Sheffield. He believes fears around accountability on individual staff are misplaced and a duty of care would actually create a legal avenue to hold those who have failed to fulfil their role.
He said: “There is an unfounded fear that universities will be sued when things go wrong. In my son’s case, there was a systemic failure, not a failure of individuals, and we think this will usually be the case.”
Ms Calvert-Lee agrees and believes the legislation the petition demands would, in fact, present an opportunity for universities to invest and “reorganise their processes and hire whatever staff they need”.
However, those concerned about the petition don’t believe this will actually happen through a legislative mandate.
A spokesperson for AMOSSHE, a student services organisation which will be attending the Committee Petition evidence session on May 16, said: “It is our view that increased funding for student mental health services in the NHS is a greater priority than an additional duty of care on universities.”
Instead, critics of the petition believe the proposals will not result in more mental health professionals being hired, but rather a heavier burden on existing staff.
Rachel Moss, a senior history lecturer at the University of Northampton, took to Twitter to voice her concerns.
The one point critics and supporters of the campaign agree on is more funding is needed, to acknowledge the pressures higher education staff are already under.
Mr McCarthy said: “If universities say they’re struggling then we must take that on board. We have to listen to what they are saying, and we have to respond accordingly.”
Another concern surrounds privacy and the way mental well-being problems are communicated to the families of those who are struggling.
Mental health practitioners are often reluctant to share sensitive and private information when university students are over the age of 18.
It is accepted professionals are not refusing to share information regardless of the situation, what advocates are calling for is a lower threshold to retain such information.
Mr McCarthy said: “I don’t think it’s as complicated as some people make out — I think where life is at risk, then we look at the next of kin.
“It’s too late when somebody has died to say that at least they have a right to privacy.”
Practically, there are also concerns over the way statistical information is treated in the case of student suicides as universities are not required to hold this kind of information on student suicide.
In a sister petition to the #ForThe100, which never gained the required 100,000 signatures for it to be debated in parliament, advocates of "Harry's Law" have called for the introduction of new rules which would see coroners informing universities when a case of suicide is recorded and publish the data annually. The petition was created after Harry Armstrong Evans, a 21-year-old from the University of Exeter took his own life.
This point could be discussed at the parliamentary debate next month, but concerns have been raised regarding the significance of such data. More specifically, due to the number of suicides being statistically low, especially when it comes to individual universities, a yearly comparison would be hard to measure.
Advocates have pointed out, though, there would be other ways of measuring the success of duty of care.
The Higher Education Policy Institute (HEPI), for instance, suggests success could be easily measured through data which reveals fewer overall students requiring support.
The stigma around mental health and suicide
Although the approach to how suicide should be handled by universities is debated, both advocates and sceptics of the petition agree that it is important to mitigate the stigma around suicide and promote dialogue.
Lisa Ravenscroft, the communications manager at ProtectED, a Code of Practice and accreditation scheme organisation for university standards, said: “We want students to declare if they do have mental health issues because then the university can be prepared and get everything in place.
“We know that a lot of students don’t, because they’re worried there’s a stigma and people aren’t going to understand.”

Strokes in Young People
Young stroke survivors from across the UK have been speaking out about misdiagnosis with migraines, uncommon symptoms and delayed treatment. Now they are calling for a change in the way strokes are diagnosed and for greater awareness of symptoms in young people

Disability versus Accessibility
Disabled people in Sheffield claim the city acts as a barrier for them to safely get around. We investigate the problems they face across the city.

A Duty of Care
With an estimated 100 students dying by suicide each year, Parliament will soon debate a proposed statutory ‘duty of care’ for those struggling with mental health issues at UK universities. What could it look like, who could it help, and why is it urgently needed?

“We work so hard, just to get our dreams shattered” – players share the struggles of making it in women’s football
Juggling with the pressures of work and study while playing the game they love is a reality faced by many women’s footballers.
Ellie Sharpe, a 29-year-old goalkeeper for Doncaster Belles, has experienced these very struggles.
She said: “So many times I work from 5am until 3pm, then come home and have a nap - just so I can then survive football training in the evening.”
Sharpe, who plays in the fourth tier of women’s football, works 40 hours a week at Lidl on top of training and playing for the Belles. She is also studying for a MA degree at Sheffield Hallam University, making it hard to find time in her day-to-day routine.
She said: “My boss keeps telling me, you need to retire from football now! ‘You need to step up to being a shift manager.' Why do you need an education?’ I just look at him and go, ‘I want to better myself’. But yeah, it’s hard juggling everything.”

Ellie Sharpe in action for Doncaster Belles. Photo credit to Doncaster Belles.
This isn’t just a struggle exclusive to those in the lower levels of the women’s football pyramid. Bex Rayner, who has played at England Under-21 level, began by playing in the boy’s team at local side Bradford Park Avenue.
Her career path saw her play for Leeds United Women and Doncaster Belles, before settling in the Sheffield United women’s set-up as a main player.
Despite the Blades experiencing success in the FA Women’s Super League 2, they remain a part-time team in a league of full-time sides.
One league off the top flight, Rayner and her teammates have anxieties not relevant to the male equivalent level.
She has had to juggle the same issues voiced by Sharpe; working in order to continue playing the game both footballers love.
Rayner said: “It’s tiring having to fit everything in and still make sure you maintain focus, fitness and quality when you get to football.”
The route to get where she is today at Sheffield United hasn’t been straightforward.
Rayner’s time at Doncaster was abruptly cut short when the Belles’ financial situation at the time meant they couldn’t be promoted to the Women’s Super League (WSL).
She said: “I think after that my motivation got knocked a little because we work so hard, just to get our dreams shattered I guess. That was tough to take.”

Bex Rayner celebrating in a Blades shirt. Photo credit to Sheffield United Women's.
One player who will be featuring for a WSL team next season is Liv Clark. The former University of Sheffield student managed to break through professionally with Bristol City and also gained international recognition with Wales.
Now fully professional at Bristol, she is still aware of the struggles faced by many footballers to get to a certain level and the dedication it requires.
She said: “When I first joined Coventry United in the Championship, I didn’t get paid expenses. So, I was paying to travel from Sheffield to Coventry four times a week as well as being a full-time student. That was always difficult.”
Another financial anxiety for women is a lack of protection when it comes to long-term injuries, a situation Belles’ keeper Georgia Wattam has experienced first-hand.
Going down with a potentially career-ending injury after rolling her ankle in training - which could result in detached ligaments without surgery - the Belles keeper has resorted to fundraising online to cover the significant costs to be able to play again.
Without additional funds, her career could be in jeopardy at just 24 years of age.
Clubs competing in the Women’s National League - the division which Belles currently play in - receive no assistance when it comes to insurance for players.
Belles’ chief executive Russ Green believes that this will continue to hamper the women’s game, with girls fearing an injury scare could end all their hard work.
He said: “Unfortunately we have another situation where the lack of support from the authorities for players at our level is laid bare and Georgia has been put in an incredibly difficult position.
“Situations like Georgia’s are preventing women coming into - and more importantly staying in - the game. Severe injuries hamper people’s ability to work their regular jobs and players are taking that into account. If those in charge of the women’s game are serious about growth, they must address this issue and provide more support.”
For some, however, making it in the women’s game never comes to fruition.
Molly Ashman was an Aston Villa academy player, the lifelong 21-year-old Villa fan’s dream. Yet, even at Academy level, the pressure was too much for Ashman to handle.
She said: “There were times, multiple times in multiple teams where I've thought, like, I don't want to do this anymore because I want to go out with my friends.
“Obviously school gets in the way as well. I just would never have time to do my homework. I'd have to tell teachers, if they wanted it the next day, ‘I just can't do that because I've got training’.”
Ashman’s dream came to an end when Villa didn’t have a development squad to accommodate her. The likes of Doncaster Belles are also on the verge of scrapping their respective development team, a worrying trend made by clubs to cut costs.
Ashman’s final match at Academy level was an emotional one.
She said: “We used to run across the pitch at the end and it really hit me. That was my last match for Villa. And I just remember I just started crying in front of everyone because it just overwhelmed me. And it was just, wow, like that, seven years has just come to an end.”

Molly Ashman playing for Aston Villa. Photo courtesy of Molly Ashman.
Although many footballers like Rayner, Clark and Sharpe, have experienced hurdles, their continued dedication and graft has allowed them to get where they are today.
With all the positive press about the women’s game continuing, it’s important to keep incentivising girls to get into the game to stop any aspiring footballers falling to the wayside.

Bereaved families of students who died by suicide to give evidence at Parliamentary committee
Grieving parents are preparing to tell their stories to the nation’s MPs at a government committee next week in a fight to get a duty of care enshrined in law.
The evidence will be given to the Petition Committee, a parliamentary group which will go over the contents of a petition submitted by campaign groups #ForThe100 and The LEARN Network.
This is ahead of a debate at Westminster Hall on June 5 which MPs will attend and voice their support in order for it to be passed to the next stage of the legal process.
One of the families attending is Dr Mark Shanahan who lost his 22-year old son Rory while he was studying at the University of Sheffield in 2018.
“We want the law to have teeth,” Dr Shanahan said. “This is not something that is going to finish on June 5. Think of Everest. We've got to base camp so there is a long way to go.”
MPs who have spoken in support of the petition include Helen Grant, the MP for Maidstone and the Wield who joined The Learn Network in delivering the petition to Downing Street ahead of the debate next month. Conservative MP Caroline Nokes was also present.
Other MPs such as Darren Henry for Broxtowe, attended the event after the petition was handed in where the families of those who had lost their loved ones to suicide at university read out testimonials.
Sheffield MPs, Olivia Blake and Paul Blomfield as well as Andrew Western for Stretford and Urmston were also at the event.
A spokesperson for Matthew Western, the Labour MP for Warwick and Leamington, said: “Matt is aware of the campaign and has met both campaign groups in Parliament and elsewhere. He will be the Shadow Minister responsible for responding to the debate on 5 June.”
Professor Edward Peck, the government’s first Student Support Champion, said in relation to the time it would take to put the duty of care into legislation: “18 months to two years to do all of what is in training around student mental health, some changes much sooner.”
In response to the petition, the government said: “Higher education providers do have a general duty of care to deliver educational and pastoral services to the standard of an ordinarily competent institution and, in carrying out these services, they are expected to act reasonably to protect the health, safety and welfare of their students.”
Ahead of a debate next month, the Petitions Committee will hear from those involved in the petition, and representatives from charities such as PAPYRUS, Student Minds and Universities UK.
They have received more than 128,000 signatures for their joint petition which concerns the introduction of a statutory duty of care to be made a legal requirement in higher education.
Duty of care is defined by #ForThe100 as protecting students from reasonably foreseeable harm, caused either by direct injury or failing to act. It is already in place in employment law in the UK.

A game of two halves
While investment and coverage of the WSL is growing, young aspiring female footballers are being left behind. We look at the troublesome situation the women’s game faces outside the sheen of its top layer.

“What we need is a culture change”: Stroke survivor calls for tailored care after locked-in syndrome
A Rotherham public health specialist who was left unable to communicate and move after a stroke has called for changes to the way survivors and their families are supported.
In December 2021, Kate Green, 43, was taking her seven-year-old son, Stanley, swimming when she suddenly had a feeling of exhaustion come over her.
She felt an intense pain in her neck after returning home where her husband, Adam, could sense a problem.
Mrs Green said: “Within minutes I couldn’t move my arms or legs, couldn’t speak, and very quickly started struggling to breathe.”
Paramedics quickly took her to Rotherham Hospital, where she would spend the next five months in care.
From her diagnosis, Mrs Green was found to have suffered a stroke due to a bleed in the brain. As a result, she experienced locked-in syndrome, which left her awake, yet unable to communicate.
She said: “At first, I was in a coma with all those tubes and wires everywhere, and when I woke up, I could not move at all.”
One of her biggest concerns, however, was her son having to deal with the after-effects.
She said: “I think for a seven-year-old, that is quite a difficult thing to process. For a long time he thought it was his fault.”
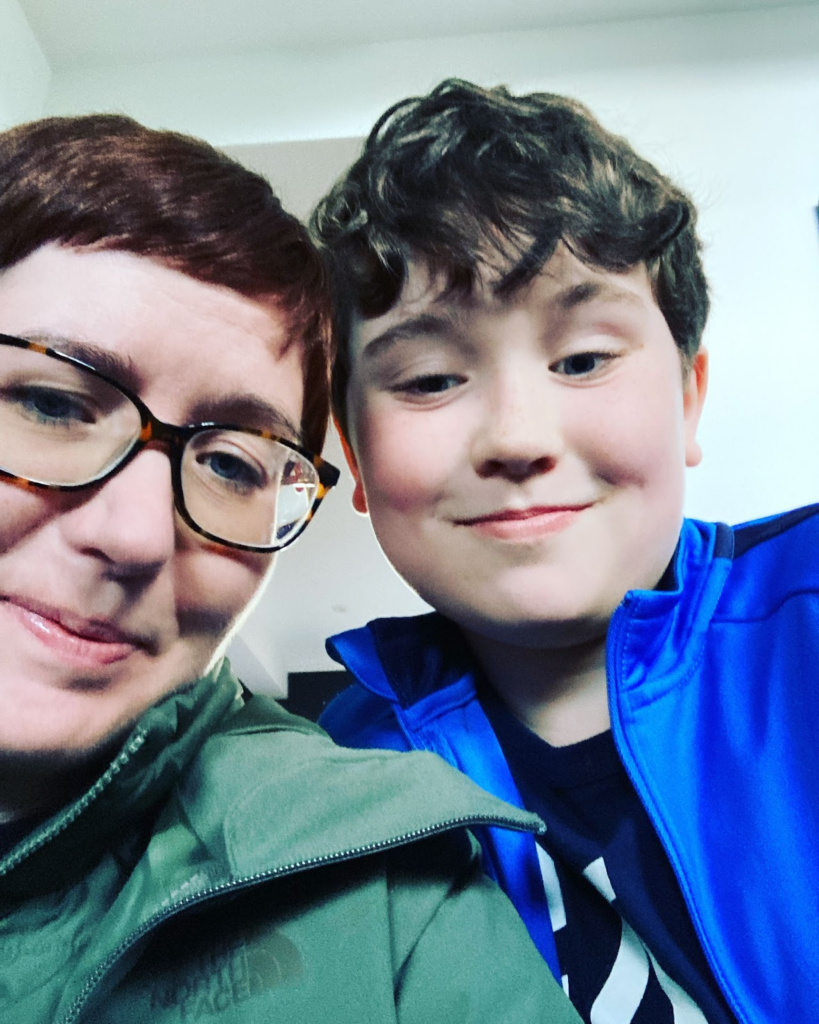
Mrs Green believes access to support for children of stroke survivors should be a basic need.
She said: “I think this sort of thing should be given out to everyone with kids automatically, some support and advice at least for them. Maybe even access to child psychologists that can help them deal through the process.”
Another issue was Mrs Green feeling she could not be in a position to receive the in-home care that was available.
She said: “In Rotherham, you carry on receiving care at home, whether that's physios or carers. But I just felt like I would not have any independence.
“Because I have a young son and a husband that works, I just felt that if I had gone home at that point, there would have been so much pressure on them to be my carers.”
Due to a lack of NHS funding for aftercare for stroke survivors, people like Mrs Green have had to pay for physiotherapy out of their own pocket.
She believes one area hospitals could improve on would be immediate access to rehab units for those without the facilities offered at home.
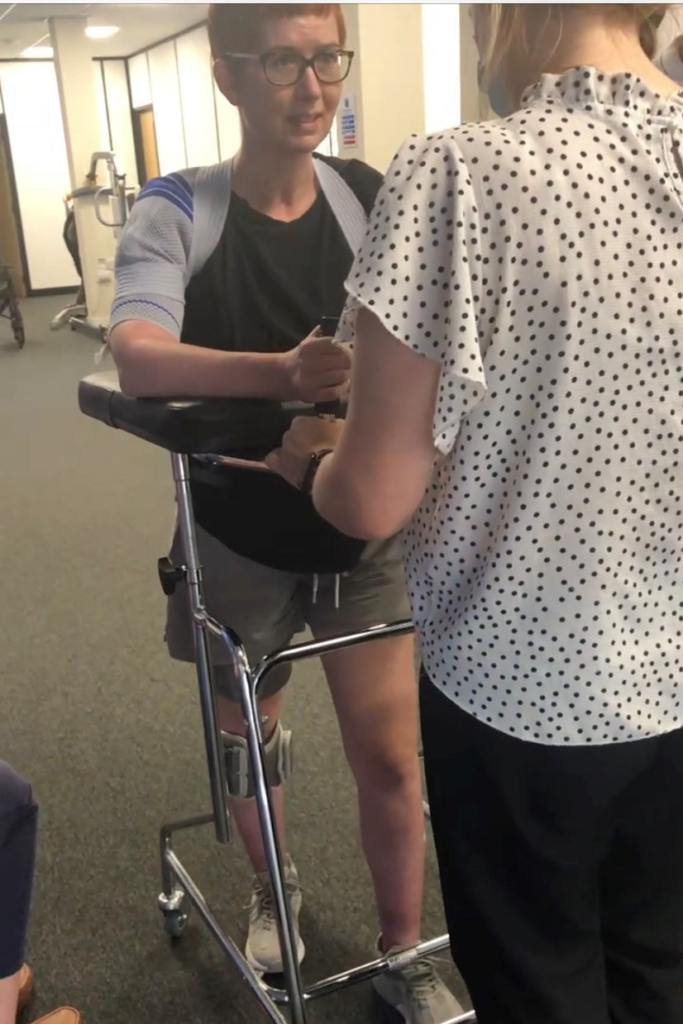
Rather than classifying stroke treatment as a form of acute care, Mrs Green thinks a better solution may be to apply a “rehab mindset”.
She said: “What we need is a bit of a culture change. I think it is the way people think about the aftercare that matters here too.”
The impact of patients leaving the hospital so soon after the event of a stroke is something Mrs Green had to face herself.
Some of the more unexpected challenges at home would push Mrs Green to fund her rehabilitation.
She said: “At first, I could not get upstairs. This definitely had an effect on my mental health when I thought I would have to sleep downstairs after saying “good night” to my family."
“I just didn't like the idea of that.”
Providing medical equipment like her functional electrical stimulation tool is another idea Mrs Green feels could be a simple, yet effective solution to benefit those making long-term recoveries.
Since her diagnosis, friends and family have said the experience was a “wake-up call”, as Mrs Green had nothing short of a healthy lifestyle before the stroke.
Mrs Green considered this a driving force behind her survival, believing a more sedentary lifestyle could have been the end.
She said: “I think I was in a better position because I didn't smoke, I wasn't overweight, and I was quite fit. I think that's the reason why I'm still here. So, I think it's so important to look after yourself from an early age.

“Even now if you had a good day of exercise, where you go to the gym for an hour a day or had a run, but you are predominantly sitting down for work, it is still classed as a sedentary lifestyle.”
While the recovery has taken time, Mrs Green has remained positive with the progress she has made so far.
She said: “My goal at the minute is just to be able to just walk around the house on my own. I feel now like it is within reaching distance. Now I can see things are getting better. I feel stronger. I think I am in a good place.”

“We can’t sit around for ten years”: father of student who took her own life on the battle for a legal duty of care in universities
“Why is nobody listening? Why is nobody understanding? Perhaps it’s too simple and so fundamental no one believes we’re asking for it.”
These are the words of Bob Abrahart, the 67-year-old father of Natasha, a university student who tragically took her own life while studying at the University of Bristol in 2018. A member of Lived Experience for Action Right Now (the LEARN Network), he is campaigning alongside #ForThe100 for universities to have a legal duty of care.
Bob believes the whole campaign comes down to a fundamental concept: people should be cared about.
The LEARN Network and #ForThe100 are two campaign groups, set up by bereaved families, fighting for the introduction of a statutory duty of care to be made a legal requirement in higher education.
Their joint petition has received more than 128,000 signatures and debated at Westminster Hall on June 5.
The campaign groups estimate 100 university students a year take their own lives, with an estimated 319 in the period between 2017-2020 in England and Wales according to a Freedom of Information request.
Duty of care is defined by #ForThe100 as protecting students from reasonably foreseeable harm, caused either by direct injury or failing to act. It is already in place in employment law in the UK.
Natasha’s story
“We discovered after Natasha’s death that, in a second-year physics module, the students had interviews. All we know from the first one-on-one interview is that she ran out of the room,” Bob, a former university lecturer said. “We have never had any more detail on exactly what happened. That was followed by another failed attempt at an interview. We don't know what happened there either.
“Natasha was diagnosed as having social anxiety disorder. At home and amongst her friends, you wouldn't have noticed it. It's only when she was put in some stressful, performance situation such as a one-on-one presentation in class, when she went shopping, when she went out for a meal, that’s when it caused a problem.
“She only managed to be marked on two laboratory assessments. One at the beginning, which she ran out of and one just before she died. That did not go well either. For the rest, she just got zeroes because they failed to address the problem. Did they fail her? The judge ruled they caused her death. So yes.”
20-year-old Natasha took her own life on the day she was expected to participate in an oral presentation which would have taken place in front of 40 staff and students.
“They should not have subjected her to six months of non-stop, that was in effect for her, torture. It is this torture which caused her to become depressed and it's the depression that led to the suicide and they still did nothing. They carried on regardless.
“So why did they? The answer is that they didn’t have to stop.”
A civil court ruled that the University of Bristol failed to make reasonable adjustments for Natasha under the Equality Act 2010 and the Abrahart family won £50,000 in damages.
However, the judge refused to accept that the university was negligent under a duty of care - because Bristol University successfully argued that none existed.
Natasha’s father argues that if a duty of care had existed, the university wouldn’t have subjected her to the distress associated with the oral assessments that she was struggling with.

“Natasha was a wonderful daughter. She was methodical in everything she did,” the former associate professor at the University of Nottingham said. “She loved computer programming and was musical. She played piano and cello.
“She had one thing holding her back: her social anxiety disorder.”
The Abrahart family are prepared to go all the way to the Supreme Court, if that is required, to get justice for Natasha. This could take up to ten years and they believe other families should not have to go through the same process.
The University of Bristol declined to comment on the matter.
UUK response
Professor Steve West CBE, the President of Universities UK and Vice-Chancellor of UWE Bristol said every life lost to suicide is a tragedy but “although universities are investing in student support and developing partnerships with NHS services, their primary role is as settings for adult learning not health care.”
“We do not believe the proposed additional statutory duty of care, beyond the existing duties that already apply to universities, would be practical, proportionate, or the best approach to supporting students.
“We question whether a compliance-led approach will drive the cultural changes needed to promote awareness and disclosure, conversations, and co-production – all of which are needed to act on prevention and early intervention.
“We continue to work with the government, and its Student Support Champion Professor Edward Peck, on proposals to improve outcomes for students.”
Government response
In response to the petition, the Government released a statement that says higher education providers already have a general duty of care.
“This can be summed up as providers owing a duty of care to not cause harm to their students through the university’s own actions.
“Over the last decade, higher education providers have devoted considerable resources to their student support services, and a good deal of support is now widely provided to students who struggle with their mental health.”
They point to Office for National Statistics data that shows a significantly lower rate of suicide in Higher Education students compared to other people of similiar age.
Looking forward
#ForThe100 and Learn Network met with MPs in Parliament after handing in their petition to Downing Street last month.
Bob said the debate in Westminster Hall in June will need backing from them in order to get promoted through to the House of Commons.
“I think people are starting to understand that we’re not going anywhere. We’re only going forward.”
You can find out more about The Learn Network here and #ForThe100's campaign here.

“People can sympathise but they can’t empathise”: Peer support group praised for combating isolation in young stroke survivors
A UK-wide charity has made young people feel validated through its peer support group aimed at tackling loneliness in stroke survivors.
Different Strokes is an organisation that connects young people across the country, including Yorkshire, through their shared experiences.
Being run by young stroke survivors for young stroke survivors, the charity set up its own peer-support network, Befrienders, in 2020 after finding a lot of its members felt alone in their journey.
Marketing manager of Different Strokes, Lauren Hartney, said: “A lot of young people have come to us with similar experiences of feeling isolated after their stroke. Many young people end up on wards which are full of older people, and it can be hard not to know anyone else your age who’s been through it.
“We saw this as a huge gap in support available for young people, so we set up the Befriending service to help overcome this.”

The service currently has four volunteers that offer support to other stroke survivors in a range of ways from answering questions and concerns to just having a friendly chat.
The conversations can happen over the phone, text or video call and can be as often or as little as the young person wants.
Befriender and occupational health administrator, Ailie Mess, 26, from Aberdeen, said: “As a survivor, I had a lot of support from my family and friends, but nobody had been through it.
“A lot of young people say, ‘I feel like the only young person who’s had a stroke’, so I wanted to give back to the charity and show young people they’re not alone.”
Some people who come to the charity might have read stories that have resonated with them so request particular volunteers, whilst other Befrienders are matched based on experiences and interests.
The matching process is undertaken by the Different Strokes family support officer, Genise Turnbull, who works closely with the group to ensure everything runs smoothly and is available to answer any questions should the volunteers need extra advice.

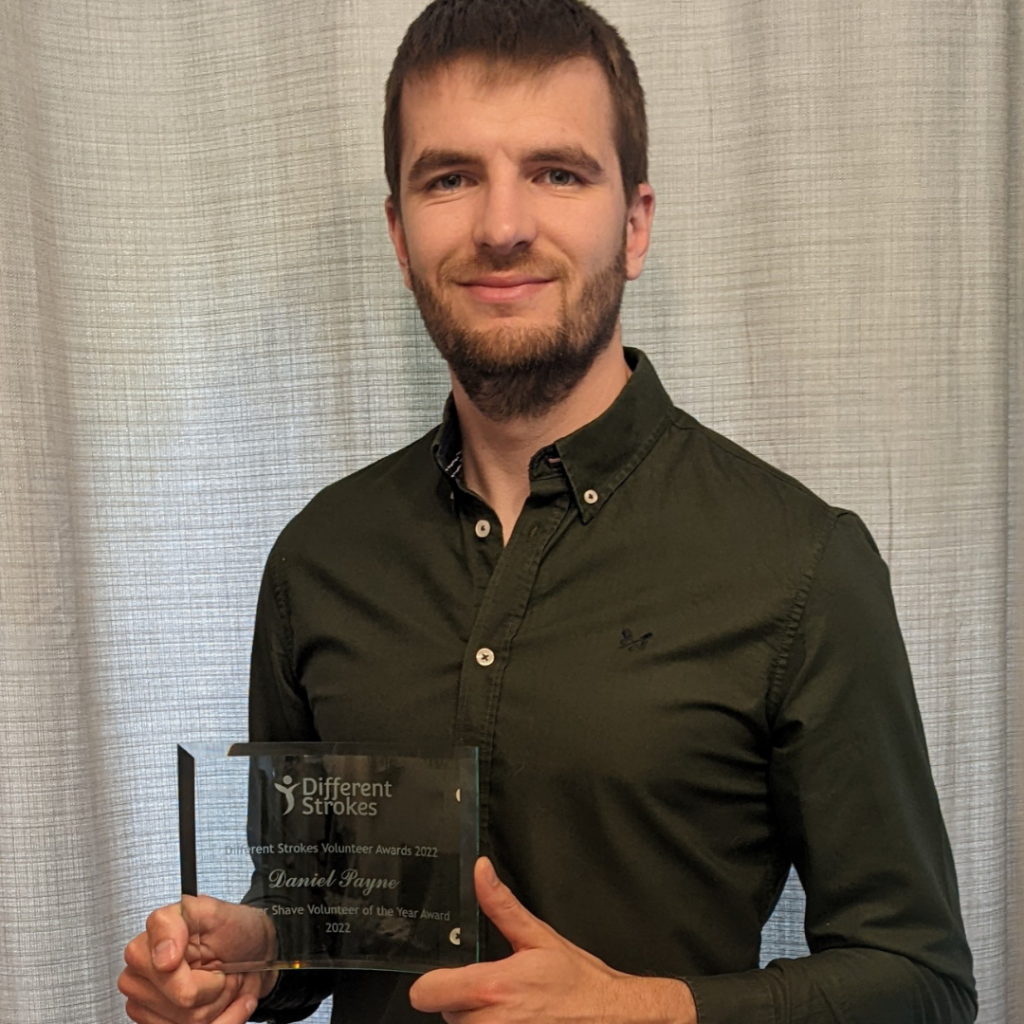
Volunteer and purchasing manager, Daniel Payne, 28, from Berkshire, said: “My fiancé works on a stroke ward and whilst she’s been amazing, it’s just not the same as talking to someone who’s also been through it. People can sympathise but they can’t empathise.
“I think it’s great being able to talk to someone who’s a similar age as it’s not just about both having had a stroke, it’s about that generational gap.
“Someone who’s older is at a very different stage in their life than someone who is in their 20s and 30s.”
The impact of the generational divide between older and younger stroke survivors is a sentiment shared by Ms Mess, who was just 21 when she had her stroke while on holiday in Iceland.
She said: “Although the matching is about age, it’s not just about matching people for the numbers.
“For me, I had my stroke when I was 21 so I was just starting out in my career having never worked full-time before. People who’ve had a stroke at 40 are still young, but they’ve already had a lot of the experiences that young people haven’t yet.”
The service is available to stroke survivors aged from 16 to 25 with many of the participants praising the validation the scheme has given them.
But the scheme has also been beneficial for the volunteers with Mr Payne, who had his stroke aged 23, enjoying being able to see the progress people make.
Mr Payne said: “It’s great seeing gradual improvements in people. It might start off with them being quite shy, but slowly people open to you and having both had a stroke, it gives you a way into a conversation.
“I can talk to people once who just need a question answered, but others I speak to on a longer-term basis where we just catch-up on general life, but from a stroke perspective, which is so beneficial.”
Although the pair are in a good position in their recovery, the charity recognises that every young person’s stroke journey can be very different.
Ms Hartney said: “Recovery isn’t linear and Different Strokes likes to keep its relationship to those we support open-ended.
“Acceptance is a life-long pursuit and whilst some will hit the different steps of their recovery and move on from the service, some will also come back and that’s absolutely fine too.”
Although everyone’s stroke experience is different, the Befrienders find that recurring points come up during their conversations with young stroke survivors.
The most common is the fatigue that many can face after their stroke as well as anxiety, navigating the dating world and feeling isolated.
Ms Mess said: “The fatigue is probably the most misunderstood and underestimated symptom as it’s invisible.
“I’ve found that other people might say to me that I can’t be tired as I’m only young, but they don’t realise I’m a stroke survivor.”

The volunteers hope by sharing their experiences, it will help other young people on their journey to recovery, and enable them to open-up about how they’re feeling.
Although it can be difficult to relive the experience of having a stroke, volunteers like Ms Mess believe that the positives outweigh this.
Ms Mess said: “Sometimes it can be hard if it’s a very similar story as it can bring up memories, but the good really does outweigh the bad and it can be so interesting and informative hearing about other people’s experiences.
“Stroke recovery can feel like going through the five stages of grief, and I wouldn’t have volunteered if I wasn’t ready. For me, it’s been a really cathartic experience and I’m so glad that I got involved.”
To find out more about the Befriending service visit the website hereFind out more about Different Strokes here

Sheffield allotments are “un-walkable, unfriendly, and inaccessible”
A resident in Sheffield has claimed that there is currently only one accessible allotment in the city for disabled people.
Norma Smith, 67, claims Burncross allotments is the only site that she would be able to use, as she is disabled.
Ms Smith regularly attends physiotherapy for fibromyalgia and arthritis, claiming it is up to Sheffield City Council to change the accessibility of allotments in the city.
She said: “Nearly all of the allotments in the city are unwalkable and inaccessible for me to get to.
“I have to get my husband to drive me to the closest possible spot to the entrance as I am unable to walk very far on uneven and dangerous paths.
“Another main issue is that most of the people who deal with the allocation of allotments are unfriendly; I am seventh on the list for an allotment but I see spare ones getting overgrown every time I go.”
Sheffield City Council state they manage over 3,000 allotment plots on over 70 sites, but with only “some” designed for disabled people.
They also say they can “create accessible plots at some sites when needed.”
Ms Smith stated the problems occurring in allotments in Sheffield include inaccessible parking, limited car space, lack of wheelchair ramps, unsafe roads and damaged paths.
On top of the existing physical issues of the sites, Sheffield City Council charges three times more for hiring an allotment than neighbouring committees such as Doncaster.
To use an allotment for the year, Sheffield charges from £80 to £100, whereas Doncaster charges around just £20.
Ms Smith claims the allotment in Hag Hill, Rivelin, has a side road that could be used, with many spare allotments going to waste as it is inaccessible for gardeners like her.
Allotments like Endcliffe Student Village are physically accessible, but are privately owned by the University of Sheffield and therefore unavailable for the public to use.
Ways to make allotments more accessible include raised beds, wheelchair friendly tables, and more seating around the site.
Sheffield City Council have been contacted for comment.
