
Beau Greaves applauded for inspiring women’s darts ahead of World Championship tie
An ex-BDO professional darts player and academy coach has shared memories of witnessing Beau when she was just a child, having shocked many players in Doncaster when playing people three-times her age.
James Thomas, owner of Next Gen Darts Academy in Beighton, is convinced that she will make a deep run at the World Championship this winter and is more than capable of beating some of the best players in the world.
He further emphasised the exposure Beau has been getting, originating from local town interest and progressing to worldwide recognition for her elite level of darts and 100+ averages that have stunned ex-professionals.
Thomas says: "I first met Beau when she was 10 -years-old. She played in the Sheffield Darts Masters and by 12 she beat a lot of the older players."
Darts academies and shops have grown amidst the sports' rapid growth, where the academy encourages girls to start playing darts, where the gap between men and women in the sport is closer than ever.
The academy has had plenty of girls come through their doors, with many looking to emulate Beau's current achievements, reaching new heights in development whilst maintaining the importance of having fun.
He also reflected on fellow female professional Fallon Sherrock, who was the first woman to win a game at the World Darts Championship in 2019, believing that Beau will soon follow in her footsteps.
Thomas says: "Anyone that knows Beau knows that she is special. It's no surprise she is where she is now."
When asked about the importance of more women's darts events being available, he told us that the Junior Darts Corporation had their first ever Women's World Championship this year, with a lot of good things to come in Ladies' darts.
The importance of women's development is vital to him, sponsoring 15-year-old darts prodigy Taylor Field, who is the 13th in the World Darts Federation's U18's women's rankings and 79th in the UK and Ireland in all ages.
Thomas says: "There's a pathway for the women's game that there wasn't before".
The three-time women's world champion and youngest ever female player at the tournament is playing in her second PDC World Championship, looking to make a run after beating Luke Littler in the World Youth Championship last month.
She has set the women's game alight this year, earning a PDC Tour Card after winning 13 Challenge Tour events and finishing second on the Winmau Development Tour.
She has been drawn against Northern Irishman Daryl Gurney on the 19th December, which will be a welcome challenge to her, facing a key figure within the sport that has won PDC titles and participated in the Premier League.

‘Brutal’ art exhibition puts people in the shoes of the homeless
A Sheffield-based charity has highlighted the city's homelessness crisis by drawing attention to the realities of rough sleeping.
The Archer Project has been running the Concrete Dreamz exhibition at Bethel Chapel on Cambridge Street from 28 November and it ended today.
The exhibition, created by design agency the Black Eye Project, shows beds made of concrete slabs, highlighting the harsh reality of living on the streets.
The beds are accompanied by statistics and experiences of homelessness during winter, asking the general public to put themselves in Sheffield's homeless community's shoes.

Joe Logan, head of fundraising at the Archer Project, spoke about the importance of the exhibition.
He said: "Not everyone has experienced homelessness. But most people have experienced going shopping, shopping for mattresses, and it's something people value and rightfully so. What we're trying to do is put it into the context of something people take for granted."
With the exhibition closing today, Mr Logan spoke about public support the project has received.
He said: "Reaction has been really positive. A lot of people have commented on how brutal it is, but people have been very kind about talking about the work we do to support."
The Archer Project has helped more than 1,100 people this year, providing warm beds and meals for 30 years.
The exhibition didn't use any lived experience of Sheffield's homeless, but Mr Logan talked about the impact of the charity's projects.
He said: "The reactions we've had from people we've supported has been varied. One that means a lot to me is someone that thought we were taking the mick out of people sleeping rough, then he visited himself, he said that he got it and he was happy about what we were doing."
The project also ran a carol service today, where poetry was shared about the struggles the homeless face during winter.
Volunteer Abby Walmsley said: "Winter is one of the toughest times of year."
The Archer Project doesn't receive any government funding, running solely on donations.
For information, or to support the project, visit Supporting Sheffields homeless and vulnerable | Cathedral Archer Project

Ten-year-old boy taking on charity walk for animal charity
A boy is tackling a charity walk in the last two weeks of December to raise money for a non-profit close to his heart.
Harry Lee, 10, is setting off in support of Pet Pals GC this December, as he aims to raise money by taking on the Winter Walk the organisation hosts every year.
The challenge sees people cover 25km across the month of December.
The time span given to do it means people of all mobility levels can get involved and raise money.
Harry and his family have been fostering dogs from Pet Pals GC since November last year, and even adopted their own dog, Astoria, from the organisation after the "kids fell in love with her."

Harry's family is incredibly pleased with how the community has come out to support him, having already raised £100 of his £150 goal.
Harry's mum, Heidi Lee, 39 said: "He's really delighted by it all.
"It's amazing how people we don't even know have been donating."
Harry has been eager to raise money in any way he can, sorting through second hand items to sell.
Louise Baker, president of Pet Pals GC, has said: "To learn that younger generations like Harry are getting involved is amazing.
"All fundraising is essential for non profit organisations like mine," she said.
The money will go towards Pet Pal GC's move to a more well-suited location, where they hope to avoid constant costs of damages to their current venue.
Harry said: "I wanted to join in because I love that the animals could have a new home to live where it's better for them.
"I also want to make it better for Louise because she already does so much hard work already and she must be very tired all of the time and sad sometimes too."
To read more about Harry's fundraiser and donate follow the link here.

Allotment rent increases branded “unacceptable”
Members of Sheffield's allotment societies have expressed concerns about the council's support in the wake of recently announced rent increases.
From next January, allotment rents will increase by 2% across plots in the city, a rise the council says is in line with inflation.
Members of Hangingwater Allotments in Fulwood have claimed Sheffield's rent charges are too high, and passionately believe a system similar to Leeds City Council would be better where rental charges are linked to the value of land as opposed to Sheffield's pricing model which takes into account land prices and water and labour costs.
In Sheffield, the biggest plot available is 301 square metres, and costs £143.10 a year, compared to Leeds where the biggest plot of 250 square metres costs £81.

Members complained about lack of support from the council, claiming the water on the allotment site was shut off for two months as council workers were unavailable to fix the problem.
With 30-50% of rent going toward water costs, members felt this was "unacceptable".
However, members of Woodseats Allotment Society welcomed the role of the council in managing their site, even declining to become independent as the group found the council's involvement more convenient.
But Woodseat allotment users also said council support had declined in recent years, with site security and management causing issues.
Sarah, 64, is a retired nurse who has managed her plot in Woodseats since 2013 and is involved in the society's activities, from working on charity events to helping set up starter plots and the society hub.

She said: "I am very happy and grateful to have the opportunity to work on the allotment and generally communication is effective."
However, she also said "there has been a deterioration in services offered," as rangers have been stretched too thin, meaning the society has taken on more responsibilities from the council such as sub-contracting to remove asbestos.
Hangingwater members claimed the number of rangers had dropped to just five across the city, while the quality of repairs had worsened and required more work.
Sheffield Wire approached the council for comment.

Plaque commemorates firefighters on the 85th anniversary of the Sheffield Blitz
A memorial to the eight firefighters that lost their lives during the Sheffield Blitz has been unveiled in Pounds Park.
The German bombing operation, code name "Crucible", destroyed much of the city centre and damaged nearly 80,000 homes, taking the lives of at least 660 people in 1940,
Matt Nicholls, Secretary of the Fire Brigade Union in South Yorkshire, paid his tributes at the service.
He said: "In 1940 when Sheffield endured the devastation of the Blitz, Norman, Alfred, Arthur, Fredrick, Stanley, Tom, John and Albert - I say their first names because they were ordinary people - met those nights with resolve."
The plaque revealed today at noon was organised by the Fire Brigade's Union, whose campaign memorialises the service of firefighters across the UK by placing a red plaque at the sites where they lost their lives in the line of duty.
The service was attended by active firefighters who had to leave the afternoon's speeches to respond to an incident.
Nigel Kind, Chairman of the National Association of Retired Firefighters, served as a firefighter for 40 years and now researches the history of the fire brigade.
Mr Kind said: "it's just showing that their sacrifice isn't going to be forgotten, we remember them like the military.
"When everybody was sheltering, these guys were out when the bombs were still falling, putting fires out and protecting the city.
"That's the sacrifice they made."
Also among today's crowds were families of the firefighters. Patricia Wyatt's uncle, Arthur Moore, lost his life on the night of the 12 December 1940.
Mrs Wyatt and her family travelled from across the UK to see the service.
She said: "He was 28 years-old and he was engaged. His ashes are now in the grave of his fiancée in Burngreave cemetery.
"We never knew him. But he was one you'd have liked to have known."

Sheffield Tribune writer handed prestigious prize by Jeremy Vine at British Journalism Awards
A writer for the Sheffield Tribune has come out on top at the 2025 British Journalism Awards, winning the prize for Best Local Journalism.
Mollie Simpson, best known for her work revealing "bribery and fraud" at the University of Greater Manchester, was awarded the prize alongside Mill Media founder and Editor of The Mill, Joshi Herrman.
Yesterday evening's annual awards night was hosted by journalist and presenter Jeremy Vine and held by Press Gazette.
The three pieces which won her the coveted title were written when she was at The Mill in Manchester.
Earlier this year she joined The Tribune, another Mill Media publication founded by former Sheffield Star journalist Dan Hayes.
The judges called Ms Simpson's work "a tenacious and first-class piece of investigative reporting by a journalist who would not be thrown off the trail.”
In an exclusive comment, Mr Herrman said: "We're incredibly excited to win this award.
"This investigation has been a story we've covered all year, and it's led to a police investigation, several mentions in parliament and the suspension of the vice chancellor and other senior university officials.
"Having it recognised with a national award is a lovely bonus," he said.
Mollie joined The Mill fresh out of university in 2021, and has since helped shape the regional media landscape across the north of England through her work in Manchester and Sheffield.
Mollie Simpson added on her own celebratory LinkedIn post: "Thanks so much to all my Mill Media colleagues for their support, and to Press Gazette."
Image: Press Gazette/Adam Duke Photography

Sheffield councillor calls for South Yorkshire to “buck the trend” on apprenticeship funding
The Mayor of South Yorkshire has been urged to prevent the abolition of a training scheme which underpins the region's economy and industries.
A council motion has requested Oliver Coppard makes Sheffield an outlier against government plans to scrap funding for Level 7 apprenticeships on 1 January.
Cllr Robert Reiss proposed the motion to take over funding of the scheme, which is a practical-based scheme that equates to a Masters degree and allows candidates to gain work experience alongside a qualification.
Cllr Reiss has a personal connection to the proposal as he works for Speciality Steels Ltd. in Stocksbridge, a company that has a history of taking on apprentices.
The new change to the funding structure would mean only those under 22 will be eligible to receive subsidy for their qualification, a group currently representing only 7% of the people who took up Level 7 apprenticeships last year.
Cllr Reiss said: "These are really important people that at some point in their working life either want to improve their skills, they want to reskill, or they want to have a bit of a change of employment and training."
Architecture, insurance and medical technology are all industries that rely heavily on the apprenticeship scheme.
The medical technology industry has been particularly outspoken in their opposition to the change, with several industry leaders such as AstraZeneca, Adelphi and Roche coming together to pen an open letter to the leader of the House of Lords, Baroness Angela Smith.
They argue: "The Level 7 Medical Statistics Apprenticeships was created to remove barriers to postgraduate education in a field where a Master's degree is the minimum requirement for entry-level roles, with some roles requiring a PhD.
"Medical technology is a crucial part of clinical trial and research, an area that the UK is a world leader [in]."
Cllr Reiss argued that this was another reason why it was so important for South Yorkshire to "buck the national trend".
He said: "You've got this labour government who said 'we've got this plan for growth, we've got this plan for change', and then you go around and do this."
The South Yorkshire Mayor has yet to address whether any change will come within the next few years.
But with a history of championing apprenticeships with initiatives such as The South Yorkshire Apprentice hub, which looks to add 300 apprenticeships to the region, there is hope that South Yorkshire can be an outlier against the change Cllr Reiss stands against.

Sheffield pop-punk sensation headlining in their hometown as part of UK tour
Pop-punk act X2 Fast will headline in Sheffield today on the second stop of their debut tour.
The "Nothing but Numb3rs" tour celebrates their two-year anniversary, in collaboration with many other bands in the area.
The first stop of their four-day itinerary was in Nottingham, the first time they ever performed in the city.
Guitarist Simon Fairbanks praised the atmosphere of the night, and called it a "high-level stage" for a Thursday evening.
After their initial success, the five-man band will return to their home base of Sheffield for the second night.
They arrived home at around 1am, but had little rest before going into the next gig, as most of the band members had to return to their day job early in the morning.
Despite the physical fatigue, Mr Fairbanks said they will have more energy for the Sheffield show, not just because of "not having to work the next day."
He said: "I think we're a lot more excited for this one, obviously, hometown head headlining. We will probably play a longer set as well, so we'll have a few more songs in there.
"We haven't decided on the exact set list yet, but depending on the length of songs we pick, probably about 13 songs."
Guitarist Harry Kilmartin said it had been difficult recently to choose which songs to play at the gigs, and usually it depended on which were played recently.
He said: "Back then we had to learn four or five different covers but we're kind of at the point now where we've got enough of our own tracks that we've got plenty to choose from, so we can be more selective with the set."
However, fans can expect to hear at least one unreleased track from the upcoming EP, following the early successful releases of "For the Better" and "There's a Last Time for Everything."
Mr Fairbanks said: "We did play a new one yesterday, but we might play a couple because we've got more time to fill the set out."
The show will take place at Yellow Arch Studios on Burton Rd around the Kelham Island area.
Doors will open at 7pm and X2 Fast will headline the event after opening performances from Wrex, Stay Safe and Wnsdy at 7.

Four weeks of strike action at the University of Sheffield comes to an end
A student-staff rally took place at Sheffield Student's Union on Friday 12 December, marking the end of a prolonged period of UCU strike action at the University of Sheffield.
David Hayes, President of the UCU Sheffield branch and a senior lecturer in Law, spoke about how the rally is a “great opportunity to hear what’s going on for staff and students.”
He said: “We are fighting against job cuts and increasing workload and the reduction of the quality of education.”
Industrial action took place in protest of compulsory redundancies, excessive workloads and cost-cutting.
Mr Hayes feels staff "are being asked to do more and more and more, with less and less and less." He is particularly concerned about the quality of education on offer.
Students, who are already battling high tuition fees in a cost of living crisis, faced 16 days of interrupted teaching.
Green Party councillor Brian Holmshaw spoke at the rally, representing the University's ward of Broomhill and Sharrow Vale.
“I am here to support this meeting, a united front against the proposed cuts to staffing and against the closure of the undergraduate and postgraduate courses," said Mr Holmshaw. “We are against cultural vandalism of removing University courses."

The University has been in regular dialogue with UCU to try to find a resolution to the dispute and have made a number of offers to try and avoid industrial action.
One anonymous student said: "I am terrified about the future of my course."
The offers included a commitment to making no further compulsory redundancies for an extended period of time.
UCU members have not yet accepted these offers and continue to take strike action and 'action short of a strike', including refusing to mark assessments outside of their official working hours.
Recently the University of Nottingham announced the suspension of entries into language courses, further concerning UCU members who worry the risk of redundancies is only getting worse.
In April, the University of Nottingham also announced more than 250 non-academic roles could be cut, with the vice-chancellor saying it was "grappling with significant financial challenges."
The current mandate for strike action began on 30 September and will last for six months.
More on this to come.
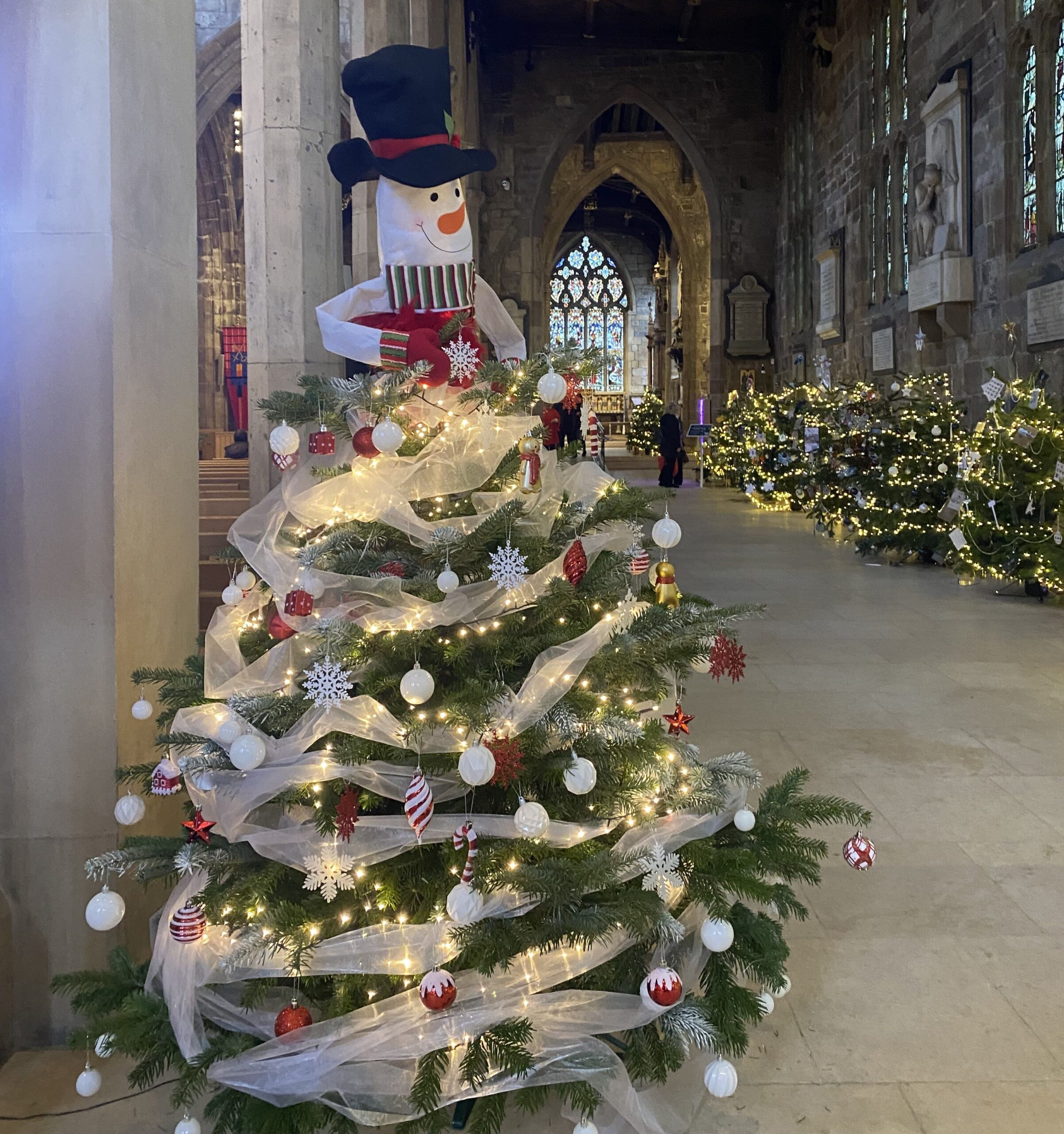
“It’s such a nice surprise to see them”: Christmas tree festival lights up Cathedral and enchants visitors
The annual Christmas tree festival has returned to Sheffield Cathedral, with more than 40 trees on display.
Each has been decorated by a local charity or community group, and sponsored by local businesses.
Visitors are encouraged to vote for their favourite, with the winning organisation receiving a £250 prize as a donation to help support their work.
The organisations, whose trees each have a distinct and vibrant theme, include the Women's Institute, Melanoma Focus, and the Sheffield Royal Society for the Blind (SRSB).
Rae Drury, who suffers from a degenerative eye disease, was drawn to the SRSB tree because of how colourful and bright the baubles were, before she realised that some were her own handiwork.
A keen crafter before her diagnosis, Ms Drury had donated her decorations to a tabletop sale at SRSB, and had wondered why they were not for sale there.
She said: "I had no idea they would be on the tree, and I suddenly thought, 'I made that'.
"It's such a nice surprise to see them, I'm so glad I can see them."

SRSB has been helping Ms Drury on her diagnosis journey, as she is predicted to become partially-sighted, and then blind, despite undergoing laser eye surgery last week.
She said that the work they do is "life-changing", and that the support that she has received, and continues to receive on her journey, is invaluable.
Some organisations have chosen to use the festival as a chance to spread information and awareness.
The Women's Institute (WI) on Ecclesall Road has decorated their tree in support of their national campaign Bystanders Can Be Lifesavers!
This campaign is targeted at spreading knowledge and understanding of CPR, and advertises free online training.

The sign written by the WI next to the tree read: "Our tree is decorated with hearts made by our members to remind us all how we can help each other by learning about CPR."
Many of the other trees also have a topical theme, with the Stop Violence Against Women tree decked in orange ribbon and tinsel, as part of their wider Orange the World campaign.
Each tree is accompanied by an informative sign, with many also including a QR code that allows people to donate, learn more, or follow the organisations' social media.
The festival is free to enter, and is open until 11 January 2026.
Art exhibition for “kind and loved teacher” draws to an end
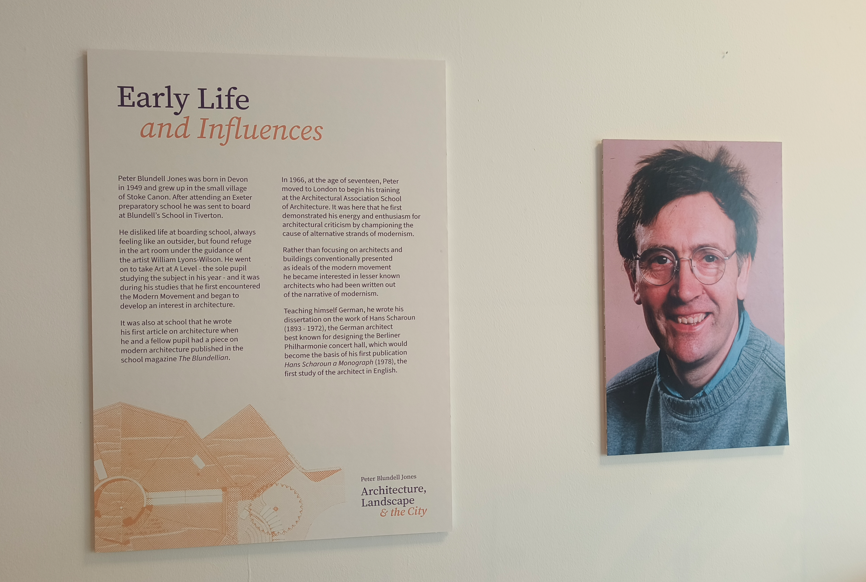
An exhibition at Western Bank Library to celebrate a prestigious architecture teacher is coming to an end after a successful six months.
Western Bank library's latest exhibition, titled: 'Peter Blundell Jones: architecture, landscape and the city', will be coming to an end on December 14, having run since July.
The exhibition celebrates the life and work of Peter Blundell Jones, an architectural historian who worked at the University of Sheffield as Professor of Architecture from 1994 until his death in 2016, when his works were donated to the University archives.
While Blundell Jones wasn't a practicing architect, he worked on architecture projects throughout his whole life, which was reflected in the exhibit.
It displays some of his notes, books, plans, models and even tools. The showcase begins with some of his work from childhood, when he was just discovering architecture, to then move onto his work as a lecturer and plans he developed in his own time.
Visitors can also watch a film, which is projected during their tours. There is also the opportunity for guests to design their own buildings.
Mariam Yamin, a senior archivist in the Special Collections heritage and archives team at Western bank library, who curated the Peter Blundell Jones exhibition said: "We've been really happy that lots of people have done that so they've really interacted with the exhibition, which is something we always hope."
The exhibition was organised with the help of the University's school of architecture and landscape, and it includes some projects done by then-students.
The biggest project, which Ms Yamin referred to as "the star of the show" is the Sheffield 1900 model, and what according to her has attracted the most external attention to the exhibition.
It was created in the 1990s by fifth year Sheffield architecture students, supervised by Blundell Jones, as a replica of the city as it would have been in the year 1900.
Featuring two train stations, and a church where the now peace gardens stand, the card and paper model shows a very different city at the heigh of industrialisation, before its landscape was changed by two world wars.
This was Ms Yamin's first time curating an exhibition. She said: "It was quite a responsibility to produce an exhibition as I never met Peter.
"He was such a kind and loved teacher. I hope he would have liked this."
The exhibition has been well received by Blundell Jones' friends and family. His widow, Christine Paulson called it a "fitting tribute."

“Britain’s favourite artform”: Yorkshire’s theatres saved by pantomime
A BBC report released this morning shows that Yorkshire and Lincolnshire theatres gained between 9% and 45% of their annual income from pantomimes last year.
James Harrison, 32, has been Musical Director at Sheffield Theatre's pantomime for the past six years.
He said: "We have regulars who always sit in the same seat, in the same place. It’s tradition and I love to be part of that.
"Gone are the days of people thinking that panto is a bit rubbish because we prove that it doesn’t have to be."
The BBC report also shows that theatres have seen a 4% increase in audience numbers from 2019 to 2024.
Simon Sladen, 39, Chair of the UK Pantomime Association, explained that panto is many children's first theatre experience, adding to its sentimentality.
He said: "Since Covid, the longing to be together has strengthened this Christmas tradition for many people, and introduced a new one for people who might not have gone before."
Mr Sladen dubbed pantomime "Britain's favourite artform," with over 260 put on around the UK each year.

Jill Ellis, 57, a teacher at Hunter's Bar Infant School, said the school takes its entire student body to the Sheffield Lyceum panto every year.
She said: "It is a tradition, but I think it's popular because it's a tradition.
"The kids look forward to it because we do it every year and their older siblings will have talked about it. It’s a shared experience."
Mr Sladen explained how pantomime supports the local economy beyond just theatres, providing learning outreach or volunteering projects with the revenue.
Local shops and restaurants can also benefit from a pantomime coming to town.
Mr Sladen said: "We’ve just had a big research project which showed that the capacity at pantomimes across the country is over 80%.
"The 2025 season is great and the respect pantomime is getting is growing."
