
Hong Kongers and allies hold pro-democracy rally in Sheffield
Pro-democracy demonstrators have been campaigning in the Moor today, following the sentencing of 45 democracy activists in Hong Kong.
Protesters are angry over the sentences as well as the British government’s lack of response, with one accusing them of looking to “kowtow to the Chinese Communist Party”.
45 activists were sentenced on the 19th of November under China’s National Security Law, or NSL, which introduced crimes of secession, subversion, terrorism, and collusion with foreign organisations.
In practice, these laws have been used to silence prominent advocates of Hong Kong’s independence from the Chinese government.
Another core issue for the protesters is the prosecution of Jimmy Lai, a British citizen and media tycoon who founded Next Digital and Apple Daily.
Lai's media outlets widely covered pro-democracy protests in 2019 and 2020, leading to his arrest under the NSL in December 2020.
Protesters view the NSL as a violation of the 1984 Sino-British Joint Declaration, which outlined that Hong Kong’s social and economic systems would go unchanged for a span of fifty years.
So far, Keir Starmer has been reluctant to speak out against the sentences. The Prime Minister recently stressed the importance of maintaining a “strong UK-China relationship” at a meeting between the two at this year's G20 conference.
Starmer also spoke of the importance of an open dialogue with Beijing over what he exclusively referred to as ‘differences’.
However, he has so far refused to openly condemn the sentencing, both at a press conference at the G20 and when called upon to do so in Parliament on the 19th of November
Asked about events in the region, organiser Clara Cheung said: “We are really angry that the UK government refuse to condemn the Hong Kong CCP government about killing freedom of expression and jailing all our friends in Hong Kong.
“We are inviting more locals in Sheffield to acknowledge it, we are also inviting them to write to their MP and tell the Labour government to keep British dignity in hand”.

Hillsborough local businesses launch new Christmas market to bring the community together
Local businesses in Hillsborough are working together to put on a new festive market at Towsure to bring about community and Christmas spirit this weekend.
With concerns that Sheffield’s main market is beoming commercialised, good tidings are being brought beyond the centre to support local businesses and communities.
Councillor Martin Smith, Chair of the Economic Development and Skills Policy Committee, said: “Markets will give a massive boost to local traders and businesses who are able to sell and showcase their goods.”
This event has been organised by a family-run business, Holme Lane Deli, together with a local pub, The Masons Arms.
Lindsey Kirk from Holme Lane Deli said: “We want to bring the community together.
“After covid, people are struggling to get back into society.”
Conscious of how the cost-of-living crisis is affecting families, the market has been purposefully planned around pay day.
With this in mind, children aged 12 and under will receive free gifts from Santa’s Grotto, donated by Towsure.
Ms Kirk said: “Kids are missing out on stuff because they’re unaffordable at the moment.”
There will be rides, a bar, a hog roast and stalls by local traders.
There will also be fundraising activities to raise money for Sheffield’s Children’s Hospital to ensure that the spirit of giving is at the forefront of the celebrations.
Towsure, which started in Sheffield as a small family-run store itself in 1967, are supporting local traders by hosting the event tomorrow and Sunday.
A Towsure spokesperson said: "It's a wonderful opportunity to bring the community together and support a great cause while celebrating the festive season."
The organisers hope that families can make memories together and that that the event will encourage people to socialise again.

EXCLUSIVE – Interview with Willis Marshall, Lib Dem councillor-elect, coming soon
Sheffield Wire is pleased to announce that we have secured an exclusive interview with Willis Marshall, the Liberal Democratic candidate for the Woodhouse by-election.
Marshall, 19, is a student at the University of Sheffield, who beat Reform UK's Andy Hizzard by just 10 votes in yesterday's election.
More updates to follow.

She Sings Sheffield: New music event provides platform for female musicians
She Sings Sheffield, a live music event for exclusively female performers showcasing their original works, was held for the first time on Monday.
The concert took place on the 25th of November at the Water Bear Live Room, and was organised and performed by four female students.
After such a successful year for women in music, with artists such as Charli XCX and Sabrina Carpenter dominating the charts, they wanted to replicate this on a smaller community scale.
One of the organisers, Alice Ede, said they hoped that the event might inspire more women to join the music industry. She said: “It’s important because women aren't given that platform when they’re starting out.”
Alice went on to talk about the extent of male-dominated line-ups in the music industry. She added: “It’s really important that we give the push for younger and upcoming artists and celebrate women.”
Another organiser expressed concern over the lack of female students on her university course. Music student Savannah Dion, speaking about the event, said: “I feel like it's much needed. We really hope to bring change.
“This event tonight gives women a place to feel safe and do what they love without fear of being judged.”
The event attracted an audience of around 30 people. One audience member said she felt the show “gave a very good message”.
Another performer, Josephine, said: “We put this event to share our music to other people but also other women to help encourage them to do the same.”
The musicians behind the event said that all the performers and audience members enjoyed the show and expressed their hope to hold similar events in the future.

“The area is being starved” says Gleadless Valley residents.
Despite repeated promises to regenerate Gleadless Valley, residents have spoken of their frustration that the deprived ‘area has stayed the same’.
Sheffield City Council allocated £83m in 2018 for the housing regeneration of the area but the funds still haven’t been used.
Despite the need for fast action, the council only managed to finalise the masterplan at the end of August 2024, switching to a community led approach, prompting locals to ask how the funds will benefit the area.

Gleadless Valley was built in the 1960’s and comprises of roughly 4,600 homes, half of which is social housing. The area has been classed as one of the most deprived estates in the country, with an above UK average of unemployment.
Two ex-members of the Gleadless Valley Tenants and Residents Association (GVTARA), Dave and Trevor, who asked not to be fully named, spoke about the area’s key issues and their concerns that locals feel are not being heard.
Dave, 67, who has been an area resident for around 20 years, said: “Crime and anti-social behaviour are a big problem and its only getting worse. The other day I saw a group of big, young, lads go into a shop and help themselves to drinks, then just walk out.”
The crime and Anti-Social Behaviour (ASB) rates in Gleadless Valley are 1.5 times higher than the Sheffield average, with the Herdings, Ironside and Plowright areas having approximately 250 incidences per 1,000 residents.
Trevor, 68, said local amenities are being neglected. “There’s no buses running up and down the road now, the number 11, they’ve axed that,” he said. “Now we’ve got to walk half a mile to get a bus. The area is being starved. Some people of our age are not mobile, they can’t get out. The government gave us bus passes but there’s no buses.”
Dave and Trevor agreed that despite the council’s surveys and data collection, things have only got worse, and the community is being ignored.
In a 2017 survey, 40% of residents living in council owned flats in the area described the state of their home as ‘bad’ or ‘very bad’. “I’ve heard lots of reports of damp and cold,” said Trevor.
Dave, who explained his home has problems with damp, has tried to speak to the council about the issues, said: “I’ve called them up about four times this week. I feel like I’m banging my head against a brick wall.”
The original 2018 regeneration plan documentation mentions three organisations who were involved with the creation of the masterplan and data collection in collaboration with residents, but their current position and involvement in the plans remains unclear.
Urbanism, Environment and Design (URBED), an urban design company focused on “sustainability and community-led design” was at the forefront of creating the masterplan yet ceased trading in 2023.
Anthony Everitt, ADE regeneration’s director, the firm in charge of funding and economic concerns for the plans, said the company has “not been involved since the original work was completed”.
BDP architects were unavailable for comment.
The council which recently switched to a community led approach, is leaning on volunteer and charity organisations to identify and rectify community issues.
Sylvia Martyn, 59, has lived in the area for 30 years, and is a volunteer at a local library and assists in community projects.
“It’s alright them saying community led but who do they mean by that? They wanted volunteers to take over the library, but it meant having a management committee who would be responsible for finances. A lot of people don’t want that.
“There are plenty of groups going on, there’s an organisation called the Heeley Trust. They come in a couple of days a week with link workers, they help people sort out benefits and signpost them to other places.”
The Heeley trust is a charity that has been working in the Heeley and Gleadless area for the last 25 years. They focus on improving the wellbeing of residents, preventing personal deprivation and improvement of public spaces.
Ms Martyn feels ASB is an ongoing problem for the area. “There are a couple of street wardens who come round sometimes but not often,” she said. “Whether they’re having any effect, I don’t know.”
She doesn’t wholly blame the council for the lack of change in Gleadless Valley. “When the right to buy came in all those years ago, the council were allowed to use the proceeds to build more houses. They wanted to raise council tax. But they weren’t allowed to do it.”
Government funding for council was stripped back under the conservative leadership. Councils are now facing a funding gap of more the £2 billion next year.
Sheffield Wire approached councillors, including the chair of the Housing Policy Committee, the chair of the South Local Area Committee and the Ward for Gleadless Valley, but they were all unavailable for comment.
As the issues with the Regeneration Masterplan delay continue, the council will surely come under further scrutiny as to their future action and spending.

Sheffield runner raising awareness for child sexual abuse at Percy Pud’s 30th annual run
Thousands will be raised for charity this weekend, as South Yorkshire's most popular 10k run returns.
The Christmas themed 'Percy Pud 10km' run was set up by the running club, Steel City Striders in 1993 and occurs on the first Sunday in December.
The 30th edition of the Christmas themed fundraiser was due to take place last year, but was cancelled due to bad weather. It will now take place this Sunday.
Katy Scott, Sheffield, ran her first Percy Pud in 2022 whilst dressed as a Christmas Pudding and will be taking part in this year's race in the same costume to raise money for The Lucy Faithfull Foundation which work to prevent child sexual abuse.
She said: "I feel quite lucky that I picked the Percy Pud for my first 10k. I remember just running along and to my left was a Santa and on my right were matching elves.
"There was music, chariots of fire and Christmas tunes blaring out from the pubs as we passed, and I was just carried along on this big happy cloud.”
As well as prizes for the top finishers in five age categories, every participant wins a Christmas pudding, inspired by a pre-war local runner named Percy who attributed winning his first race on Boxing Day to eating a whole Christmas pudding the day before.
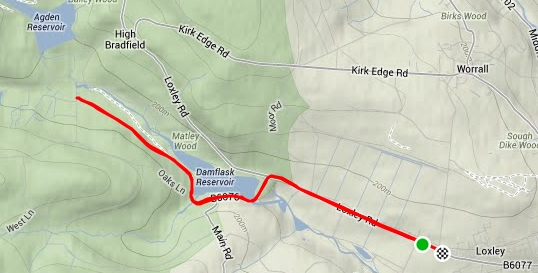
The race starts and finishes on Loxley Road and takes participants around the outskirts of northwest Sheffield.
So far Katy has raised £1300 out of her £2000 goal for The Lucy Faithfull Foundation, which protects children and supports individuals and families who have been affected by abuse.
She said: “The charity means a huge amount to me, and I am very proud to be raising money for and to be talking openly about this cause.
“Had I been more aware about child sexual abuse, 30 years ago, when my two children were young, perhaps I could have prevented my own daughter from being sexually abused for four years as a child from someone within our own family. Or at least I could have recognised it was happening and stopped it.”
The Lucy Faithfull Foundation also offers help and advice for parents and carers and supporting individuals and families who have been affected by the abuse.
They work with Stop it Now who have an anonymous helpline for anyone with concerns about child sexual abuse.
Katy said: “I find other charities, perhaps ones that make us feel less uncomfortable, seem to get a lot more public airtime. People are just very uncomfortable talking about child sexual abuse. For me, to prevent child sexual abuse, we need to start talking about preventing it.”
Katy and her daughter, who is now an adult, are now openly comfortable talking about this and on Sunday, Katy will be running alongside her daughter and sister who she describes as her “main cheerleaders."
You can donate to Katy's fundraiser via the link: https://donate.giveasyoulive.com/fundraising/katys-first-10k-race

Black Friday online sales threaten Sheffield businesses’ Christmas profits
Black Friday means big business for online giants such as Amazon, but small businesses at Sheffield's Moor Market feel like they can no longer compete.
Last year Amazon’s Black Friday and Cyber Monday sales amounted to $170 billion dollars. They accounted for 18% of the entire Black Friday sales and this year, Amazon’s profits are predicted to rise again.
Independent business owner Mintar Basi, who runs Men’s Streetwear Store MINT in Moor Market, said “every year Black Friday kills us, everyone's looking for online deals”.
The shop originally opened in 1990 and relocated to Moor Market last year.
He knows his independent business is not the only one feeling the impact of Black Friday, saying: “The highstreets struggling in general, this year the footfall is declining”.
There is huge competition between online retailers and Mr Basi feels small in-person retailers are not given an equal chance to turn a profit over the Black Friday weekend.
He said “It's dog eat dog out there especially when you’re competing online. It’s just not a fair playing field”
Mr Basi thinks in-person shopping should not be undervalued. Speaking about Moor Market he said “This is a community hub, we are like a big family under the market umbrella. We get a lot of the older people coming through, it's definitely a social place too”.
The risk of online shopping over Black Friday weekend is increasing. Last year online scams rose by 29% over the period.
In an effort to protect people from bogus websites and calls, Doncaster Trading Standards have issued a clear warning to shoppers looking for a bargain.
“If it's too good to be true it probably is. Be aware of fake texts and emails about delivery or calls from scammers pretending to be Amazon trying to get bank details”.

Richmond’s Tree of Hope switch-on sheds light on the importance of community
The Saint Catherine of Siena Church in Richmond is gearing up to host this year’s Tree of Hope light switch-on event later today.
What started as an attempt to boost the local residents’ morale during Covid19 in 2020 has now become a yearly tradition, attracting people from all over the ward. The event has been especially well received by people who feel isolated in the area.
The event is funded through the East LAC Richmond Ward Pots which the local councillors allocate. The Tree symbolises not just the beginning of the festive season but alludes to a wider sense of community and a collective aspiration for a better future.
The event is about giving people from all walks of life a place to come together, talk, make new friends, listen to music and go back feeling good.
It focuses on the rising issues of loneliness and isolation in the community, and aims to give people who are struggling a platform to connect with someone who might be able to help.
While talking about the event, the Councillor for Richmond Ward, Diane Hurst, said: “[It] might be held on Christian premises, but it's secular. It's not linked to any particular faith.
“[It] came out of community group meeting inspired by the community, and everybody is welcome to attend”
In the past, the event has seen community organisations put up stalls to inform people of various initiatives available, recruit new members and raise funds. This year is going to be no different, with free food, Santa’s grottos, and wreath-making activities all available.
The first tree was a small "fairybell tree’" and has been upgraded over the years. This year’s tree is bigger and programmable – with the ability to display patterns and play music.

The location of the tree also has been strategically chosen so that everyone can see the tree and what it stands for while passing by.
Councillor Hurst explained: “It's on the corner of a road, and it's very visible.
“So for everyone that goes by on the bus, as they walk into the shops, as they're walking home or drives by, they can see it as a symbol of hope, and the lights can shine out at the darkest time of year.”
The event will start at 4pm today and lights are scheduled to be turned on at 5:30pm.

Strange cloud formations spark the imaginations of the people of Stocksbridge
A local man spotted UFO- shaped clouds while walking in Stockbridge this morning.
Grant Hudson was walking on Yew Trees Lane at 8am today when he spotted the two giant clouds over the north of the city which he thought looked very similar to an alien invasion force.
Mr Hudson said:
“I thought they were weird and looked like flying saucers. There were two that I could see. I often take photos on my iPhone and compile them into books and these are a part of a set I sell on my website.”
Library-shop | England | Clarendon House Publications


Photo By Mr Grant Hudson - Looking West while walking around Bolsterstone.
After sharing these unusual photos on social media, people took to the comment section and jokingly wrote that it was an alien invasion force while others expressed their admiration for Mr Hudson's rare capture.
These strange cloud formations are called “Lenticularis” and according to the Weather Channel are one of the main leading causes of UFO sightings.

Photo By Mr Grant Hudson - Looking West while walking around Bolsterstone.
These formations happen when air travels over a tall object like a mountain and the air is forced to rise over it, forcing the air to spread and dip making a UFO shape in the cloud.
If you would like to learn more about these strange phenomenon's, follow the link to the weather channel to learn more. Nine of the world's rarest cloud formations and the science behind them | The Weather Channel

Kim Leadbeater shares former Sheffield MP’s story in favour of the Assisted Dying Bill
The Assisted Dying Bill is being voted on in the House of Commons today and was first proposed by Labour MP for Spen Valley, Kim Leadbeater.
She has addressed the Commons saying that the current option for terminally ill people wanting to end their lives is to travel to another country.
She said: "It is often deeply distressing and very lonely experience, shrouded in secrecy, with people feeling like criminals."
Ms Leadbeater explained that approximately 600 terminally ill people take their own lives each year. She spoke of the experience that former MP Paul Blomfield had when his dad, Harry, was diagnosed with inoperable lung cancer.
Paul Blomfield, the former MP for Sheffield Central, has tirelessly campaigned in favour of the Assisted Dying Bill after his dad took his own life, alone, in his garage in 2014.
As she spoke of Paul's experience, Ms Leadbeater said: "Harry wasn't suicidal, he loved life, but he has watched too many of his friends have lingering, degrading deaths and did not want that for himself. He couldn't tell Paul and his family of his plan as they would have been complicit and face prosecution."
"And how many precious days and weeks did Harry miss out on as a result of having to take action while he was still able to physically do so?"
Mr Blomfield was the MP for Sheffield Central from 2010 until 2024, when Abtisam Mohamed took over as the Labour MP earlier this year.
Ms Mohamed has released a statement on social media stating that she will vote against the bill later on today and hopes that her constituents respect her decision.
She said: "I recognise any initial change in the law would apply only to terminally ill people, I worry that our families and society will forever be changed by it."
Olivia Blake, MP for Hallam, is still undecided.
Live updates to follow.

The assisted dying bill- what is it?
The Assisted Dying Bill, first proposed by Labour MP Kim Leadbeater, is being voted on today in the House of Commons. With many MPs being undecided on which way to vote, it is expected to be a tight decision.
MP Kim Leadbeater became the MP for Spen Valley in 2021. She is the younger sister of Jo Cox, former Batley and Spen MP, who was murdered in 2016.
The bill allows people to make the decision to medically end their lives if they are terminally ill and over the age of 18. Candidates for assisted dying must also have been registered with a GP for at least one year, have the mental capacity to make the choice, and be excepted to die within six months.
It would excludes people with disabilities and mental illnesses.
The patient must have two separate witnessed declarations and two independent doctors to sign off on it. Then the application would have to go to a high court judge, who will ask to hear from at least one of the doctors and will make the decision.
If then approved, the individual must self-administer the medication needed to end their life. It has also been made clear that they can change their mind at any stage.
Assisted dying legislation already exists across the world, in countries including Switzerland and Spain.
In England and Wales, the bill is being voted on today in the House of Commons. MPs have been given a free vote on the issue, meaning they can vote how they wish without influence from their party.
Some MPs have publicly stated how they are going to vote ahead of today.
Abtisam Mohamed, MP for Sheffield Central has said on social media that she will not be supporting the bill and will vote against in today.
She said: "I am concerned that some of the most vulnerable people in society, low-income or disabled people would feel like a burden to others, and it would encourage them to give up."
It has also been publicly opposed by the Secretary for State for Health and Social Care, Wes Streeting.
However, Clive Betts, MP for Sheffield South East has stated that he will be voting in favour of the legislation as he believes we need to respect the wishes of those suffering from terminal illnesses to decide how they die.
It is expected to be a tight vote, with a lot of MPs still undecided as of this morning.
There will be live updates to follow.

