
“They go above and beyond”: Charities in South Yorkshire finally receive the recognition they deserve
Written by Madeline Avery and Lysia Wright.
The unLTD Business Awards have announced the shortlist for their Not for Profit Organisations Award 2025 recognising charities around South Yorkshire.
The nominated organisations are Parson Cross Community Development Forum, the Roundabout Youth Homeless Charity, South Yorkshire's Community Foundation, and the Sheffield Churches Council for Community Care (SCCCC).
The SCCCC is an organisation which supplements Sheffield's wide range of social care resources, and helps people in the area with their four key values: committed, credible, compassionate, and caring.
They save the NHS £3.4 million each year through their project which helps people with transportation.
Amongst other stories of community care and touching anecdotes, Karen Redfern, operational lead for Hospital Homes mentioned how the organisation had brought a deaf and blind dog to see his owner Phillip who was in a palliative care unit in hospital.
She said: "The minute he walked in the room his little tail was going."
Ms Redfern expressed her hope that the nomination and attention will keep people donating and help them continue their wonderful work.

Another organisation, the South Yorkshire Community Foundation (SYCF), was also nominated for the award.
Natalie Harrison, the communication manager for SYCF, believes that the opportunity to be nominated for these awards plays "A crucial role in recognising achievements, motivating teams and enhancing credibility."
Ms Harrison also said that SYCF were looking forward to their 40th birthday next year and that their nomination only further solidifies the pride they feel for having awarded £40 million worth of grants in this time.

Parson Cross Community Development Forum were also nominated for the award for their dedication to providing a voice for local people.
One of their projects is a memory cafe in Parson Cross which provides support and a social space for people facing dementia and their families.
Marie Crookes, who comes with her husband who has dementia says she enjoys coming to the cafe to socialise.
She said: "I come for company for myself because we can't get out anywhere and he can hardly walk."
Mrs Crookes also emphasised how these awards and recognition for the organisation helped keep the cafe open and help people meet others in the same situation.
Howard Gordon, 63, who was diagnosed with dementia in 2017 said that the group provides him with the support he did not receive after his diagnosis.
He said: "I was given two leaflets and told to make my own power of attorney."
He said that the group is vital to the community and that he had nowhere to turn before he found the memory cafe
He praised Louise Ashmore and Louise Askew who help run the group saying: "They do so much for us, they go above and beyond."
The awards ceremony will be on Thursday 11 December when the winner will be announced.

Midday JUS News Rundown for the 28th November, 2025
Here are all the latest news from around Sheffield and South Yorkshire. Follow us on social media here:
Instagram | Facebook | YouTube

From Sheffield youth to England’s greatest, is success in Australia the final task in Joe Root’s glittering career?
The one blemish in England’s greatest Test cricketer’s career is his battle to reach that elusive century down-under, but the Chair at Joe Root's boyhood Sheffield club believes "he will come good in Australia."
Mark Longley, of Sheffield Collegiate Cricket Club (SCCC), has spoken out in support of the Yorkshire-born batter saying 'he’s done it everywhere else' and there's no reason why he can't achieve his dream in Australia.
The 2025-26 Ashes began last week, reigniting the discussion around Root, after England's painful defeat in Perth.
The 34-year-old has a staggering 39 test centuries and has topped the ICC Test batting rankings on nine occasions.
The Ashes are the only mark on Root’s career, as he is yet to score a hundred on Australian shores, with a high score of 89 from the 2021-22 series in Brisbane.
Over an international career spanning 13 years, Root has collected a staggering 13,551 Test match runs for England.
This is only topped by India legend Sachin Tendulkar's 15,921 runs, which is in chasing distance for the Sheffield batter.
The success Root has enjoyed in international cricket would not have been possible without help he secured from his home side, SCCC, supplying him with the skills to succeed on the global stage and achieve his well-deserved title of England greatest ever cricketer.
Based at Abbeydale Park in Dore, Sheffield, Root spent his junior years at the club learning his trade.
"I saw him grow up at the club," said Mr Longley. “He was always very keen and would regularly stay in the nets until beyond dark.
"Joe was an orthodox player and you were not going to get him out. Teams made it harder for him to score before he gained power and a range of shots.”
SCCC has a remarkable alumni; 2005 Ashes winning captain Michael Vaughan, international cricket umpire Richard Kettleborough, and Joe’s brother and Glamorgan player, Billy Root having all played for the side.
Longley explained there is a strong focus on developing junior players at the club, leading to high end talent being produced.
Root’s first taste of senior action came when he was just 11-years-old, highlghting his determination.
Mr Longley believes it was Root’s “hunger to learn and keep on improving,” developing his talent into becoming one of the world’s best players.
Joe Root's success as a professional
Root's success in every country apart from Australia is what undoubtedly makes him an England great. Even in Australia, his record is not terrible with nine half centuries and an average of 33.3.
However, compared to an overall test average of 50.94, it is evident why pressure is being heaped onto him.
Build up to the current Ashes series was dominated by negative. Headlines from the Western Australia press, labelled Root “Average Joe”.
His 15 test matches in Australia are the longest ever winless streak by an England player.
Questions have always been asked about whether Australian conditions suit Root’s style of play, and with a miserly return in the first Test match at Perth, pressure has been mounting with a less favourable pink ball match up next in Brisbane.
Sheffield's finest still holds immense influence in local community
Root's mindset has been described as “hugely professional with one of the smallest egos I have ever seen in a player,” by Mr Longley, who watched Joe grow up at SCCC.
The cricketer who hails from Dore still remains a huge figure at SCCC. He recently attended a club dinner to raise money for Sheffield Children’s Hospital Charity, supporting the club which elevated Root into his hugely successful career.

Mr Longley also added there is immense respect for him at the club, and when Root visits it feels like he is “just one of the dads at the bar" as nobody swamps him for photos.
As a local Sheffielder, Root grew up in the sporting arena. He attended the same secondary school, King Ecgbert's, as Olympic Gold medallist and three time World Champion Heptathlete, Dame Jessica Ennis-Hill.
Mr Longley believes “having a go the earlier the better” is important for engaging kids with the sport and potentially finding the talent.

Honest assessment required after Perth batting horror show
The current Ashes series is the perfect opportunity for Root to prove his doubters wrong and score that elusive century in Australia that has haunted him for 12 years.
On England’s Ashes chances, Mr Longley said: “England must reflect on their poor batting performance," and does not believe the narrative that head coach Brendon McCullum thought that the team scored well in the first test.
They only batted for 67.5 overs across two innings, with many describing some of the shots played as reckless.
The consensus amongst many England fans was that the performance did not live up to expectation, and denial from McCullum will only add fuel to the fire in this high stakes series.
“There are a few more twists and turns ahead,” said Mr Longley as the five match series gives him hope, adding: “Joe will deliver, I am sure of it.”
The positivity from a long-time friend of Joe provides a change from the negative thoughts echoing from the media, which are driven by England’s extremely poor record in Australia since winning the 2010-11 version.
With an away Ashes hundred and victory being the only achievements stopping Root from reaching cricketing immortality (if he is not there already), there will be the drive and determination required no matter what the approach England decide to take.
Mitchell Johnson, the former Australia fast bowler, said in The Times: “To be considered a great, you probably need to have scored a hundred in each of the main Test-playing countries.
"He knows what he’s achieved and people who have played against him know what he’s achieved, but he’ll surely be disappointed if he doesn’t make that score.”
Root's career has been on an upwards trajectory since he reached his 30s, averaging 56.11 since the beginning of 2021.
His adaptability is displayed from opening the batting for England when he broke into the team, to finding his suited position at number four later on in his career.
So, maybe it's still a tad premature to label England's greatest cricketer "Average Joe".

Yorkshire Foundation takes Santa to people’s doors this Christmas
The founder of a Yorkshire-based business has started a Santa Van initiative for those who cannot leave their homes to see Father Christmas this festive season.
Beverley Maw started her Occupational Therapy business this April after 23 years in the NHS, and just three weeks after starting up the business created the BMOT foundation to continue a lifetime of giving back to the community.
Ms Maw said: "I've done lots of charity work in the past, I've created charity evenings and always liked things like that.
"I almost felt guilty for not working in the NHS anymore, so I just wanted to give something back."
BMOT has a variety of patients and clients ranging from those with speech and language difficulties to children who are in palliative care.
The charity's Christmas initiative has seen Ms Maw turn her own Campervan into a mobile Santa's grotto to spread the festive cheer.
The Santavan will be making its maiden voyage today (November 28). The scheme which was initially established to spread the fun and festive joy across Yorkshire, has now expanded all the way to South Shields.
Ms Maw has said the initiative is just about "having some fun, and making people smile" but there is a greater impact behind the initiative.

The Santavan ready to spread festive cheer
Stacey Gorton, a support worker whose workplace is due to receive a visit from the Santavan this weekend, said: "It will give our individuals enjoyment seeing the Santavan as we can't always find somewhere to take all of our individuals as a group to see Santa as we work with autism and challenging behaviour.
"The impact this will have will be a massive achievement to our service and our individuals as a group and seeing their joy makes it all worth while."
The Santavan will also provide gifts to the people it visits. The making of the presents has been a real family affair.
Ms Maw's mother, who is 81 and recently took up knitting as part of her rehab after breaking her shoulder last year, has been knitting therapy BMOT bears as presents to help those who suffer from anxiety.
Sadly, while the initiative has received a lot of requests and applications, there have been insufficient donations so far, resulting in Ms Maw having to fund much of the project out of her own pocket.
If people wish to donate then they can visit the link: Meet Santa! - Beverley Maw Occupational Therapy

Supertram apologises to customers for recent delays and cancellations
Amid complaints about poor punctuality and suspension, Supertram has handed out apology leaflets to the passengers waiting for the tram at main stops around the network this morning.
The message acknowledged the poor performance of the tram system in the past few weeks and especially in the past few days, with cancellation to the Blue and Yellow line.
Many customers have had their daily activities and meetings interfered with because of the tram delays and disruptions, making the transport system the centre of debate on SheffieldForum.
The leaflet stated "We’ve got plans to invest over £600m to fix those problems over the next few years. But in the meantime, we’re going to do everything we can to fix what we can, hire more staff, freeze fares in the New Year, and communicate better, so when there are problems, we explain what’s happening."
In today's statement, Supertram attributed the continuous disruptions to a combination of two primary issues: substandard infrastructure following the public takeover in May and a spike in staff and driver sick leave.
But it is not all gloomy weather for the future of Sheffield's Supertram.
There has been efforts from the South Yorkshire Mayoral Combined Authority (SYMCA), including a current £110m investment, to improve the tracks and and add new stops. SYMCA is confident that will be more improvement to come.
SYMCA is determined to return South Yorkshire public transport and Supertram, in particular, back to a "world-class", reliable and, foremost, cost-effective system for the people.
South Yorkshire's Mayor Oliver Coppard said: "My mission is clear: to build a world-class, integrated public transport system and make sure it’s affordable.
"Public control means decisions that put people first. Whether you’re commuting, studying, visiting family or heading out for the night, we’re creating a transport network that works for all of us.”
Oliver Coppard is hosting a public meeting on Monday December 1st at the Showroom Workstation in Sheffield to talk about the current issues and future outlook of the Supertram.
People can join the session from 5.30pm.

Sheffield designer uses old climbing equipment to craft sustainable clothing accessories
A Sheffield designer is championing sustainability by making clothes from preloved climbing ropes.
Natalia Pearce, 38, founded Scavenger in 2012 after studying product design at Sheffield Hallam University. Her passion for both sustainable fashion and climbing led to her combining the two.
"I came across this bin for collecting climbing gear just after I'd graduated," she explained, "and I just wanted to see what the potential was for reusing the ropes and see what products I could come up with."

The wider conversation around sustainability has been rife following the Conference of the Parties annual summit, and more specifically in fashion after more brands are committing to using recyclable materials in their supply chains. Earlier this year, a report from Zalando confirmed that 74% of people want to wear clothes more sustainably.
“There’s a lot of climbing walls in Sheffield and a lot of climbers, so it’s nice to give people the option to dispose of their climbing gear in a sustainable way," Ms Pearce said. "People really enjoy seeing that their gear is getting a second life."

The unique process begins with a phone-call from a climbing centre to collect bins of used rope.
Once they are retrieved, the ropes are then sorted by colour and size, before being cut into 3-4m strips. After their cores have been removed, they are then sewn into fabric strips.
“The ropes are the building blocks for all the fabric and the products that we make,” Ms Pearce said.
It's a story that began in the attic of her dad's house, a curtain acting as the only divide between her work and home life.
Now she operates from a studio perfectly situated beside the Foundry Climbing Centre.
"I always looked across from my old studio over to here and thought it would be perfect to be here" she added.

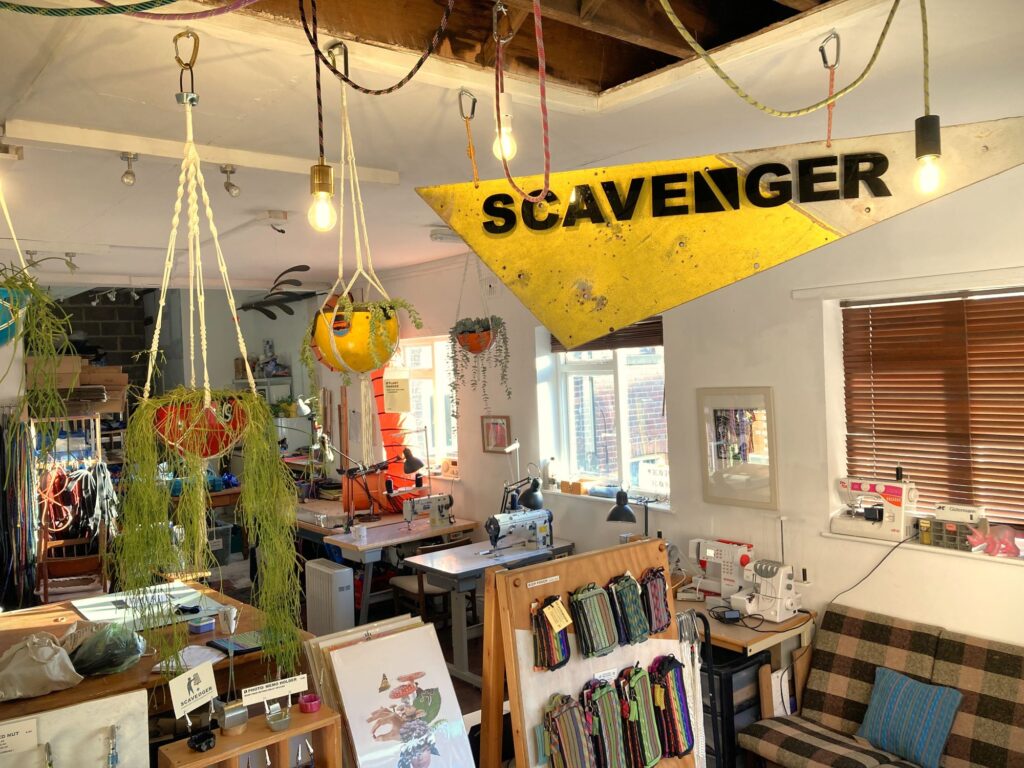
The company also collaborates with local artists and businesses often, one in particular being Hunk Print who gives vintage shirts a new lease of life by hand-screen printing them.
Scavenger will soon host an Open Studio event on the 1st of December where attendees can enjoy free hot spiced apple juice, mince pies, and giveaways.
You can also browse their selection of sustainable gifts and accessories.


Second boy bailed after shooting on London Road
A second suspect in the shooting of a 16-year-old boy has been released on bail after his arrest on suspicion of conspiracy to commit murder.
A 15-year-old boy was also released on bail yesterday.
The victim, also 16, remains in hospital fighting for his life.
Inspector Amy Mellor, of South Yorkshire Police, said: "We know that people within our communities will hold crucial information about the horrific events that unfolded on Monday."
Superintendent Martin Simcock added: "Gun crime, and violent crime has no place in South Yorkshire, and the fact that a young boy is fighting for his life is appalling and will not be tolerated.
"This boy and his family deserve answers, and we are committed to getting them," he said.
Contact police with any information on 101 or Crimestoppers anonymously on 0800 555 111.

Sheffield Wednesday Ladies take on Ilkley Town AFC
Sheffield Wednesday Ladies sit fourth in the North East Regional Women's Football League after a "really encouraging start to the season", and are looking to keep the foot on the gas this weekend.
The Owls have won four of their first six games, and are prime position to finish high in the table come the end of the campaign, should they keep up their impressive form they have shown in the early stage of the season.
Andy Gilligan, the manager of SWL, is delighted with how the team has performed so far as he said: "I've been really happy with how things have gone."
With a strong run of performances under their belts, Mr Gilligan's mantra of taking every game as it comes is how he plans to keep the team grounded.
He said: "We try to just focus on the next match and let 'runs' take care of themselves."
For the game against Ilkley Town, at the Jubilee Sports and Social Club, SWL will be without key players such as Jess Birtles due to injury.
However, with Amy Broomhead being eased back into the fray, Mr Gilligan has "a strong squad to select from".
Nicole Shaw joined the club in July 2024 from Barnsley FC, and has already scored seven goals in just nine games in the league, as she said: "I think I’ve had quite a positive start to the season".
Miss Shaw attributes her recent successes to that of her teamates, and how much it has helped to have a strong squad alongside her.
She said: "I am lucky enough to have a really good squad behind me that give the the confidence to play better and believe in myself."
Miss Shaw also sang the praises of the backroom, saying: "we are very fortunate to have such an encouraging and supporting coaching staff".
The team will need to be ready for everything that sixth placed Ilkley Town throw at them, but with their current form, and the team cohesion on display, all three points may just be coming back to S6.

Student cold water plunges in name of Movember campaign
In support of the Movember campaign, students are taking part in '30 days of 30 cold dips' to raise money for the Men's Mental Health Charity.
Various sporting committee's from the University of Sheffield have participated in a cold water jump at Crookes Valley Park on each day of November.
Women's Cricket Club Captain, Ria Gill, is one of the students taking part.
Ran by student Movember ambassador Joseph Skidmore, has helped raise funds for the charity.
Although anxious at the beginning, Miss Gill completed the jump feeling "exhilarated and thankful to support the cause".
The University of Sheffield have finished as the 5th highest fundraising University in the country and have raised over £74,000 in the 2025 campaign.
Movember are a leading charity who advocate for Men's Mental Health as well as raising awareness for Prostate and Testicular Cancer.
Money raised for the campaign has allowed them to run over 1,250 mental health projects, transforming the way in which men receive support.
The month of November allows for communities to come together and raise money for the charity.
Movember have highlighted the work of students especially: "As it stands we have almost hit £1.5m raised by UK universities this campaign, all of which will make a crucial difference in Men’s Mental Health and Suicide Prevention, Prostate and Testicular Cancer".
When asked why Miss Gill was participating in this, she stated: "I believe for us as a club it is an important cause to raise awareness of as Men's Mental Health especially can be overlooked”.
Alongside the jump, Miss Gill also participated in a charity cricket match against the University's Men's Cricket Club earlier in the month, and all together, the University's Women's Cricket Team has managed to raise over £600 for the charity.
The most prominent campaign held by the University was their charity fashion show ran by the Sports Committee, the show managed to raise £2,103.50 and had the support of 26 companies who donated food, drinks and raffle prizes.
Although one of many campaigns ran by the University, the '30 days of 30 cold dips' campaign is a substantial insight into how students are actively participating in the Men's Mental Health Campaign.
Listen hear to gain an insight on a student's take on the importance of raising awareness for Men's Mental Health.

From score to stage: Sheffield panto Musical Director does it all
After winning Best Pantomime at the UK Pantomime Awards last year, the Sheffield Theatres panto is back.
Starring BBC Strictly Come Dancing's Kevin Clifton, CBeebies superstar, Evie Pickerill and Sheffield legend, Damian Williams, this year it is Aladdin that will be taking over the Lyceum Theatre.
We went down to talk with "the most enthusiastic man in show business" James Harrison, 32, who has been the Musical Director for the Sheffield pantomime for the past six years.
While most Musical Directors are confined to the orchestra pit, Harrison has campaigned for the show's music to be included on stage with the rest of the cast.
He said: "I think most Musical Directors would argue that that is harder, because you're technically doing more work, but for me that's what makes it fun."
Paul Hendy returns as the show's writer and stage production royalty, Evolution Productions are bringing the rest of the magic.
Harrison works with them to curate the show's soundtrack and "panto-ify" the songs, he told us how he incorporates popular music, such as songs from SiX the Musical, into the score: "Finding ways of making new songs work within the context can be a challenge, but sometimes it presents itself naturally.
"A bit like last year when I changed Six to be Seven for the seven dwarfs - it was perfect."

Harrison talked about how improvisation and comedic timing are also important parts of the job: "I love it when the audience member who Damian picks on has a name that I can work with.
"Last year a man was called Ross so of course I played the 'Friends' theme tune on piano."
Without giving any spoilers, Harrison described this year's show as "very interactive" and "the funniest one yet".
Aladdin opens next week, running from 5 December to 4 January. Tickets are on sale now.
Sheffield Theatres have already announced that Damian Williams will return next year for Cinderella, and this time he is bringing his sister!

Wilder calls for “consistency” as Sheffield United face Leicester amidst busy schedule
Manager Chris Wilder spoke today about Sheffield United's prospects for Saturday's game against Leicester City, a side they have not beaten since 2008.
Wilder interviewed unsuccessfully for Foxes manager last summer following their Premier League relegation, a point heavily laboured in this morning's press conference.
Despite being "disappointed not to get that gig", Mr Wilder said the rejection "worked out fantastically", as he is happy to be back managing United.
In answer to questions about the mood surrounding this personal 'grudge' match he said: "There's an incredible amount of respect, they're one of the strongest groups of players there's been"."
Sheffield United last played on Wednesday against Portsmouth, who they beat 3-0.
The Blades have played three games in the last six days, and when asked if his side was fatigued, Mr Wilder voiced some frustration, saying they "need to overcome a little bit of a juggling act".
We spoke to Mr Wilder more about the busy schedule:
The schedule gives Leicester a slight advantage, as they last played Southampton on Tuesday, a loss that saw them drop to 15th in the table.
Mr Wilder said: "We'd like it flipped the other way of course, any advantage you can get in this division you want to take."
The onslaught of fixtures hits harder as United are missing five players thanks to an injury crisis, but despite setbacks, Mr Wilder remained positive.
He spoke highly of the abilities of new signings Jairo Reidewald and Tahith Chong and stressed "consistency is really key".
This attitude has been seen in recent results for the Blades, who squarely beat Sheffield Wednesday and Portsmouth this week.
Mr Wilder said: "This is a big challenge for us, they can produce performances if they want to."
However he also said that for teams on a "downward trajectory" like Leicester, "winning games is tough."
The sides last played each other in the 2020/21 premier league season, when Leicester won 5-0.
(Coverage of the game will be shown from 11:30 on Sky Sports +, kick off at 12:30.)
Picture credit- Sheffield United

Founding Arctic Monkeys bassist launches book with Sheffield exhibition
Backstage photos, old guitars and a Brit Award went on display in Sheffield, courtesy of a former band member from one of Sheffield's biggest musical names.
Arctic Monkey's founding bassist launched a new book as a celebration of the 20th anniversary of the band's first album, at a Sheffield exhibition last weekend.
Andy Nicholson has released the coffee table book, I Bet This Looks Good On Your Coffee Table, in honour of the Arctic Monkeys' debut album Whatever People Say I Am, That's What I'm Not.
The book features photos from 2005 to 2007 as they dealt with rising fame and their first international tours.
"There was a long time where I didn't want to look at the photos or think about it but now it's started to be a real celebration of what we achieved on that first album," Mr Nicholson told Sheffield Wire.
The idea for the book started 10 years ago when he discovered a hard drive full of thousands of photos from the early years of the Arctic Monkeys.
"I just started digging," he said. "There ended up being thousands of photos that I'd taken along my time with the Arctic Monkeys when we were on tour, and dressing rooms, and sitting around."
The photos from the hard drive were then paired with cuttings from a scrap book and boxes of magazines and other memorabilia that Mr Nicholson's mum kept in the early years of the band.
Picking the idea for the book up eight years later he chose to honour the anniversary of the band's first album, calling it "a beautiful time to do it".
The book was launched with a Yorkshire Artspace exhibition in Sheffield, featuring images from the book alongside old guitars and amplifiers, awards, old magazines featuring the band, and the cameras that made the whole thing possible.
When asked about the launch exhibition, he said wanted to give fans a more three dimensional experience to complement the pictures from the book.
Mr Nicholson left the band in 2007 being replaced by Nick O'Malley.
While Mr Nicholson made the book without input from the other members of the band, they all received a copy once it was finished.
"They all really enjoyed it," he said.
The book, which costs £40, can be ordered from Mr Nicholson's website.
