A Rotherham public health specialist who was left unable to communicate and move after a stroke has called for changes to the way survivors and their families are supported.
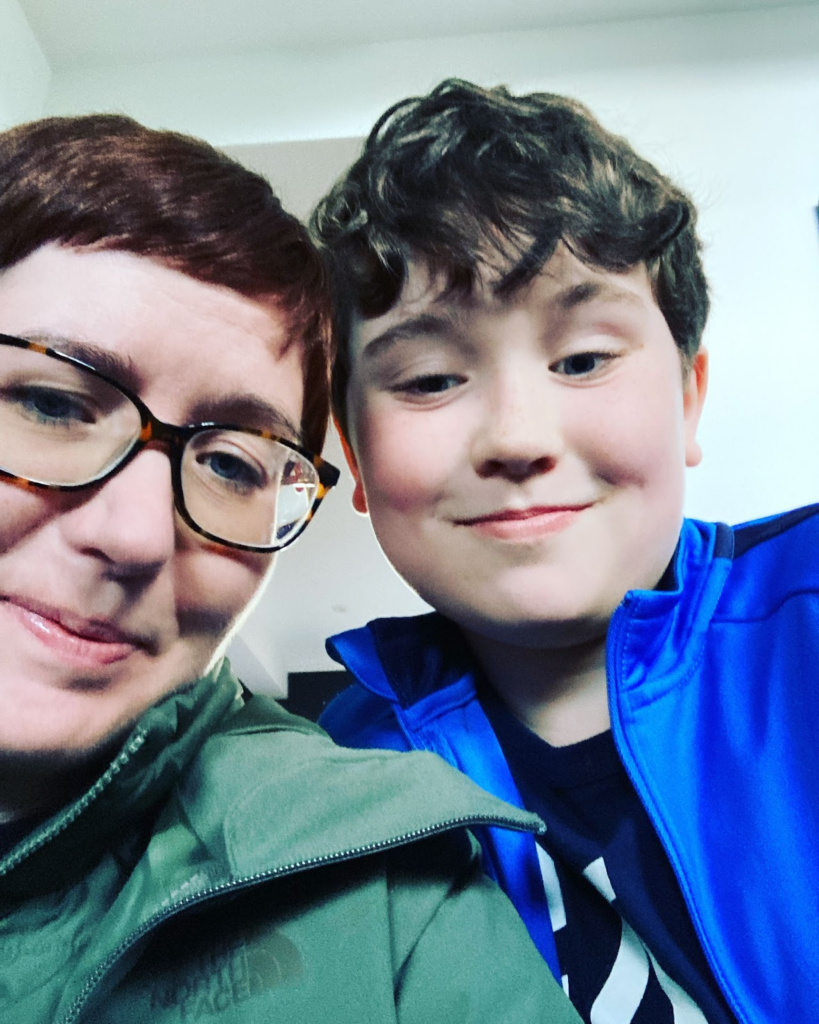
In December 2021, Kate Green, 43, was taking her seven-year-old son, Stanley, swimming when she suddenly had a feeling of exhaustion come over her.
She felt an intense pain in her neck after returning home where her husband, Adam, could sense a problem.
Mrs Green said: “Within minutes I couldn’t move my arms or legs, couldn’t speak, and very quickly started struggling to breathe.”
Paramedics quickly took her to Rotherham Hospital, where she would spend the next five months in care.
From her diagnosis, Mrs Green was found to have suffered a stroke due to a bleed in the brain. As a result, she experienced locked-in syndrome, which left her awake, yet unable to communicate.
She said: “At first, I was in a coma with all those tubes and wires everywhere, and when I woke up, I could not move at all.”
One of her biggest concerns, however, was her son having to deal with the after-effects.
She said: “I think for a seven-year-old, that is quite a difficult thing to process. For a long time he thought it was his fault.”
Mrs Green believes access to support for children of stroke survivors should be a basic need.
She said: “I think this sort of thing should be given out to everyone with kids automatically, some support and advice at least for them. Maybe even access to child psychologists that can help them deal through the process.”
Another issue was Mrs Green feeling she could not be in a position to receive the in-home care that was available.
She said: “In Rotherham, you carry on receiving care at home, whether that’s physios or carers. But I just felt like I would not have any independence.
“Because I have a young son and a husband that works, I just felt that if I had gone home at that point, there would have been so much pressure on them to be my carers.”
Due to a lack of NHS funding for aftercare for stroke survivors, people like Mrs Green have had to pay for physiotherapy out of their own pocket.
She believes one area hospitals could improve on would be immediate access to rehab units for those without the facilities offered at home.
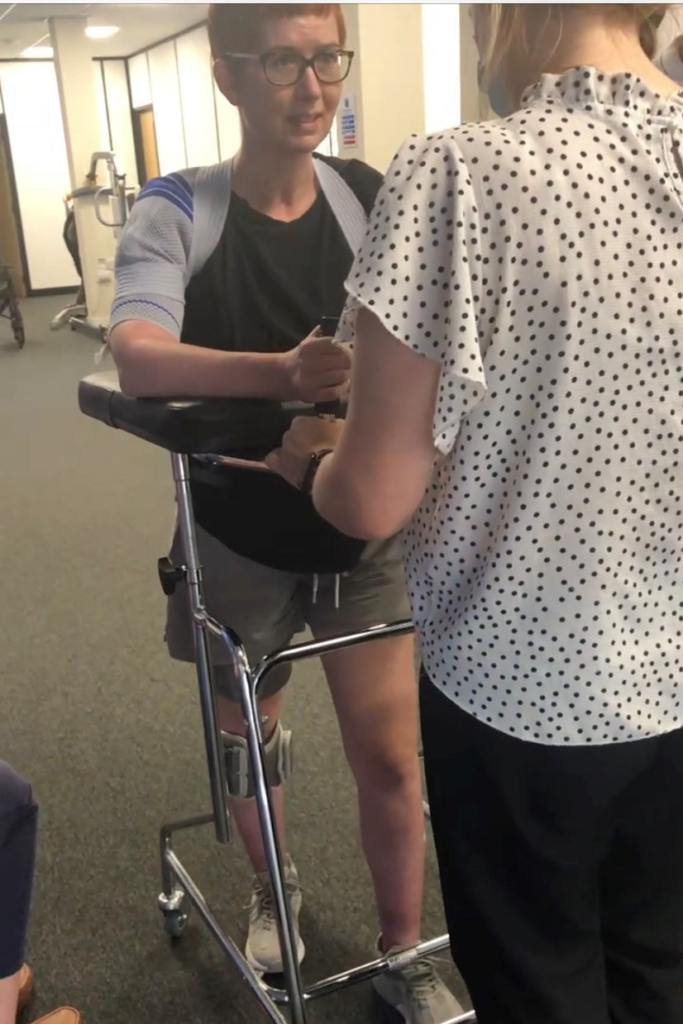
Rather than classifying stroke treatment as a form of acute care, Mrs Green thinks a better solution may be to apply a “rehab mindset”.
She said: “What we need is a bit of a culture change. I think it is the way people think about the aftercare that matters here too.”
The impact of patients leaving the hospital so soon after the event of a stroke is something Mrs Green had to face herself.
Some of the more unexpected challenges at home would push Mrs Green to fund her rehabilitation.
She said: “At first, I could not get upstairs. This definitely had an effect on my mental health when I thought I would have to sleep downstairs after saying “good night” to my family.”
“I just didn’t like the idea of that.”
Providing medical equipment like her functional electrical stimulation tool is another idea Mrs Green feels could be a simple, yet effective solution to benefit those making long-term recoveries.
Since her diagnosis, friends and family have said the experience was a “wake-up call”, as Mrs Green had nothing short of a healthy lifestyle before the stroke.
Mrs Green considered this a driving force behind her survival, believing a more sedentary lifestyle could have been the end.
She said: “I think I was in a better position because I didn’t smoke, I wasn’t overweight, and I was quite fit. I think that’s the reason why I’m still here. So, I think it’s so important to look after yourself from an early age.

“Even now if you had a good day of exercise, where you go to the gym for an hour a day or had a run, but you are predominantly sitting down for work, it is still classed as a sedentary lifestyle.”
While the recovery has taken time, Mrs Green has remained positive with the progress she has made so far.
She said: “My goal at the minute is just to be able to just walk around the house on my own. I feel now like it is within reaching distance. Now I can see things are getting better. I feel stronger. I think I am in a good place.”