With some student midwives looking after 20 mums and babies at one time, and academics saying they are underpaid, under-recognised and understaffed, many are rethinking whether they want to continue in the profession at the end of their studies.
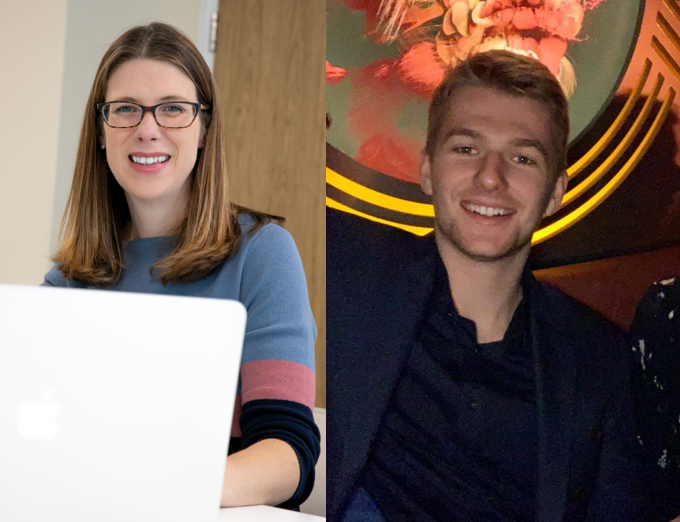
When Phoebe Gregory started training as a midwife she wanted to create families, support people and advocate for women. Now, after three years of training and placements at NHS trusts around the north of England, she is no longer sure. “Last year I was questioning if I still wanted to be a midwife,” she says.
Over the course of their degrees, student midwives undertake 2,300 hours of placements at NHS trusts where they are supposed to be shadowing more qualified staff and learning key skills. Instead, all the student midwives we spoke to said they felt like free labour.
“We do thousands of hours of unpaid work for these trusts and then don’t get a guaranteed a job at the end of it,” says Phoebe, who studies at Sheffield Hallam University.
Another midwifery undergraduate, who was too scared to be named, said even as first years, students were filling the gaps in staffing on critical wards.
“I was on a full postnatal ward, so that’s 20 women and 20 babies. It was me as a first year and one qualified midwife. That was it,” she says. “It was just horrendous.”
Shockingly, this is a common experience among student and qualified midwives. According to data from the RCM, 87 percent of midwives they surveyed said they had worked on wards so understaffed they felt unsafe.
Independent investigations into maternity wards have raised concerns about staffing levels and their impact on patient safety, but as well as these practical implications, understaffing is eroding the essential relationships between midwives and patients.
“I’ve delivered babies before where I’ve put a baby on their chest and actually introduced myself then for the first time”, says student midwife Annie (not her real name).
Another undergraduate midwife, Lara, says: “It’s a domino effect of third years being thrown into rooms, which we all hate because you can’t have a relationship with patients. You just catch their baby and don’t even know their name and then you’re off to the next delivery.”
This depersonalisation can have tragic consequences for mothers. According to Delivering Better, a campaign group who are calling for safer and more compassionate maternity care, one in four mothers have a negative birth experience. Among these, continuity of care was something many mothers felt would have improved their experience.
“There’s no substitute for a relationship between a mother and a midwife,” says Jo Cruse, founder of Delivering Better.
“Where many women are seeing a different midwife at every appointment, there are risks in terms of information being lost,” she adds.
In recent years midwives have been expected to document every decision made and score women on factors such as their BMI and risk factors.
However, rather than improving care for women, the student midwives we spoke to said ‘scoring’ women in this way can diminish their voices and lead to issues being missed.
“If you know something’s abnormal for a specific person, but it doesn’t score on the clinical factors, you can’t really escalate it very easily,” says Phoebe.
Furthermore, guidelines determine when it is recommended for people to have certain interventions.
Patients are meant to be able to decide to go ahead with birth plans outside these guidelines. However, midwives’ fears around repercussions if something goes wrong are influencing the choices available to women.
“If someone wants to give birth outside of guidelines, some midwives don’t even want to go to that home,” says Phoebe.
“They don’t want to be there. They don’t want to document anything, because they’re scared of being outside the guidelines. So if someone advocates for themselves for something outside the guidelines, they’re seen as a problem. They’re seen as tricky.”
Midwife notes can be recalled for court cases for up to 25 years after an incident and midwifery undergraduate courses like those at Sheffield Hallam University have even begun to include mock court cases as part of their training.

The Ockenden inquiry was an independent investigation into maternity care at Shrewsbury and Telford NHS Trust which found that at least nine women and 201 babies, if given a better standard of care, could have survived.
Despite the seminal impact of the following report, the student midwives say some of its key recording recommendations are still not being implemented.
One central recommendation was that after every major incident, midwives and other staff involved are supposed to discuss what went wrong, both for the mental health of staff and so they can learn from the mistakes.
Despite this, none of the student midwives we spoke to had ever had what they would describe as a formal debrief in their three years of placements.
One student midwife said: “I have been to a debrief, but it was literally having a cup of coffee 20 minutes later and saying ‘Oh, should we say this was a debrief?’, and they had ticked the box.
“That was the debrief after a woman had a hysterectomy because of her haemorrhage – a major, major incident.”
This is not because midwives do not want to learn from mistakes but that they simply do not have time to do them, says Phoebe.
Professor Hora Soltani, who teaches midwifery at Sheffield Hallam says: “Student midwives come in with so much hope and so much positivity but then they just face so many challenges: they’re underpaid, they’re under-recognised, they’re understaffed.”
She says this is leading to many questioning whether to stay in the profession.
The student midwives we spoke to are coming towards the end of their course but even those who want to stay in midwifery are struggling to find jobs.
Annie says: “I’ve applied to every single job in a 50 mile radius from my house. In two months there were about four jobs, so no one’s recruiting.
“So they say there’s no jobs because the trusts can’t afford to recruit new staff, but actually I have never stepped foot in a hospital that’s fully staffed.”
Even if they do manage find jobs, the student midwives are adamant that something has to change for them to remain in the NHS long term. Increasing caesareans and medical intervention in birth is leading to declining numbers of midwifery-led births.
Experts believe midwives will soon act more as obstetrics nurses, supporting doctor-led deliveries.
For Annie, that is not an option. “I want to help as many people as possible have a beautiful delivery,” she says.
“I don’t want to be just stood at the side, you know, putting a gown on a woman, shoving stockings on her legs without her knowing what’s going on. That’s not what I want to be a part of.”